Views: 0
Genetic Treatments for Acne May Be a Real Possibility in the Future, but None Exist Today, and None Are Currently in Development

The Essential Info
Genetic treatment aims to fix or replace defective or missing genes that cause a disease. To date, genetic treatments exist for only six life-threatening diseases, and researchers are hard at work testing genetic treatments for many illnesses that have no other cure.
However, the only treatments that have been successful so far treat diseases that are caused by a single defective gene. Since acne is a complex disease caused by many factors, including most likely multiple genes, developing a genetic treatment for acne presents a serious challenge.
Even if a genetic treatment for acne were to enter into trials, the process is a long one, so in a best case scenario, we would be over a decade away. In reality, we are likely much further away than that.
If all of that weren’t already discouraging enough, even if a genetic treatment for acne were successful at fixing or replacing defective genes involved in acne, this would probably not completely clear acne, since other factors aside from genes most likely contribute to acne, such as hormones.
However, the pace of progress in genetic research gives us reason to hope that such a treatment may be available in the distant future.

The Science
- How Gene Therapy Works
- What Diseases Are Candidates for Genetic Treatment?
- How Safe Is Gene Therapy?
- Is Gene Therapy Ethical?
- The Bottom Line
Gene therapy is a relatively new type of treatment that adds or replaces genes to treat or prevent diseases. The idea is to either fix defective genes that cause a disease or to replace them with healthy genes.1 Gene therapy is currently available for a handful of diseases and is undergoing testing for many others. In most cases, these are serious diseases that have no other cure.2,3
At this point, no gene therapy is available for acne, nor are any clinical trials underway to test future gene therapy treatments for acne. For such treatments to become a reality, scientists will need to overcome several hurdles:
- Identify genes that contribute to acne: Gene therapy can only work on diseases that have a genetic component. In other words, it is only effective for diseases that result, at least in part, from a defective gene. Scientists believe that acne is such a disease. One gene that might be defective in people with acne is called FoxO1. Normally, FoxO1 acts like a volume control button, suppressing other genes that contribute to key steps in acne development: the overproduction of skin oil, the overgrowth of skin cells, and inflammation. Scientists think that in people with acne, the FoxO1 gene might be underperforming. Another reason to suspect FoxO1 of being faulty in acne is that some acne treatments, like the topical retinoid adapalene, actually work by boosting the activity of FoxO1.4 Of course, it is likely that acne is a polygenic disease, which means that many different genes, if they malfunction, probably increase the likelihood of a person developing acne. This means that we need to identify all the genes that contribute to acne before we can develop a genetic treatment for it.5-7
- Develop techniques to fix/replace multiple genes simultaneously: Since acne is likely a polygenic disease, for gene therapy to work, scientists would have to find a way to fix multiple genes at the same time. So far, the genetic treatments that have been successful have only had to fix or replace a single defective gene. This means that technical advances are necessary before we can attempt to treat acne genetically.
- Find a way to target only skin cells: One of the main challenges in gene therapy today is how to target only the cells that play a role in a disease. For acne, this means targeting only skin cells and not, say, heart muscle or brain cells. Changing the genes in the wrong cells could result in serious side effects. This means scientists must find a way to zero in on just skin cells for gene therapy to be a safe option for acne.
- Thoroughly test any new genetic acne treatment: Changing a person’s genes can lead to unpredictable health risks. This is why any new genetic treatment must undergo rigorous testing and receive approval from regulatory agencies before doctors can prescribe it.1 This process can take over a decade. This means in a best case scenario we are still many years away from a genetic acne treatment being available to patients.
Even if scientists overcome all these hurdles, acne is still a so-called multifactorial disease.5 This means that many other factors besides genes combine to cause acne. In other words, gene therapy may help with acne but probably not cure it.
Still, there is reason to be optimistic. Cancer is another multifactorial disease involving many genes and many research groups are already testing experimental genetic treatments for cancer. One day, genetic treatment for acne may be a real possibility as well.
How Gene Therapy Works
To understand how gene therapy works, we first need to remind ourselves what genes are.
What is a gene and where does it live?
A gene is a piece of DNA containing instructions for making a protein. Proteins are the building blocks of our bodies. In other words, genes are the recipes our cells use to build and repair our bodies.
Genes come in different lengths, but all human genes live in one place in the cell: the nucleus (an organelle in the center of the cell). The nucleus of each cell contains DNA coiled into rope-like structures called chromosomes. Each chromosome is the home of hundreds or even thousands of genes.2
The Human Genome Project, an international research program that began in 1990, concluded that each human cell contains between 22,000 and 25,000 genes.2
Scientists name each gene using a combination of letters and sometimes numbers according to its function. For example, the KRT1 gene provides the recipe for our skin cells to make a protein called keratin-1.8
How genes can go wrong
Genes can go wrong in three ways:
- A gene may be missing from birth
- A gene may be defective from birth
- A gene may mutate (change) during a person’s life
Depending on the gene, some abnormalities may be harmless, but some can disrupt the production of important proteins and lead to diseases.
The goal of genetic treatment
The aim of genetic treatment is to add missing genes or to fix abnormal genes that underlie a disease. Ideally, this should restore the body’s ability to make key proteins so that the body functions correctly and becomes healthy again.
The history of genetic treatment
The idea of genetic treatment is not new. The geneticist Marshall Nirenberg, who won a Nobel Prize for his genetics research, suggested the idea over 50 years ago. At the time, he called it “gene surgery,” but scientists today use the term “gene therapy.”3
The first attempt to transfer genes took place at the National Institutes of Health, a major research institution in the United States, in 1989.3
How is it done?
Now let’s get into the deeper science of how we fix or replace genes when those genes are inside the cells of a fully-grown person. There are two ways to do it: gene therapy or gene editing.
1. Gene Therapy (introducing new genes)
The idea of gene therapy is to introduce new, functioning genes to compensate for the ones that are defective or missing in the body. In other words, instead of attempting to fix the existing “bad” genes in the person’s body, we just add “good” ones.
This sounds simple but is a technical challenge. The problem is that we cannot just inject the correct genes into the body. We need to somehow get them into the nucleus of the cells. To do that, scientists use something called a vector (a sort of carrier or delivery system). The simplest vector is a virus, because viruses are naturally good at getting into people’s cells and entering the nucleus. Of course, to use a virus as a vector, scientists have to tinker with it first so that it cannot cause illness–otherwise, the cure might be worse than the disease!1,2
The nuts and bolts of gene therapy
Although the most common vector for gene therapy is a virus, scientists can also use a synthetic (man-made) vector that will deliver the correct genes to cells.
There are also different ways of getting the vector into the target cells:
- In vivo: The doctor introduces the vector directly into the patient’s body, for example, into a vein or into the diseased organ
- Ex vivo: The doctor takes a sample of the patient’s cells, introduces the vector into those cells in the lab, and then returns the cells into the patient’s body9
Which approach doctors use depends on the disease and on the organs affected by it.
Gene therapy is currently available for a handful of diseases and is being tested on patients for many others. Acne is not among these diseases. However, just recently, researchers reported on a successful gene therapy treatment of two people with a different, severe skin disease called epidermolysis bullosa.
A gene therapy success story

An article published in the prestigious journal Nature in 2017 reported on a successful experimental treatment of a genetic skin disease called epidermolysis bullosa. This life-threatening disease results from mutations in genes that provide instructions for proteins called laminins. Laminins are important for keeping the outer layer of the skin attached to the tissues below. Patients with epidermolysis bullosa develop severe blisters and chronic wounds that are prone to infection.
In the study, a research team from Italy treated a 7-year-old boy with epidermolysis bullosa. The scientists took a patch of skin from the boy, grew the skin in the lab, and introduced a healthy gene into this skin. The cells that received the healthy gene grew into big sheets of skin. Doctors in Germany then performed two surgeries to transfer this healthy skin to the boy, covering 80% of his body with the new skin. Two years later, the body was still healthy and had not developed any blisters, suggesting the procedure may have cured him.10,11
The same year, another patient was also successfully treated with gene therapy for the same disease, as reported in the Journal of Investigative Dermatology. A 49-year-old woman with epidermolysis bullosa had been suffering from a leg wound that hadn’t healed in 10 years. The scientists took a small sample of skin from the woman’s palm, grew it in the lab, introduced the healthy gene into it, and then transplanted the healthy skin into the woman’s leg.12
2. Gene editing (repairing an existing gene)
The idea of gene editing is to repair the defective genes in the person’s body. In other words, instead of adding “good” genes, we try to fix the existing “bad” ones so they will function correctly.
Gene editing is very tricky because it requires a way of getting into the nucleus of cells, finding the malfunctioning genes among tens of thousands of other genes, and then making precise changes to just those genes–all of this in a living, breathing person. Currently, scientists use specialized molecules that work like scissors, cutting DNA at very specific places.
The nuts and bolts of gene editing
The “scissors” that scientists use for cutting DNA are called nucleases. There are currently three major nuclease systems:
1. Zinc finger nucleases (ZFNs)
2. Transcription activator-like effector nucleases (TALENs)
3. Clustered regularly interspaced short palindromic repeat (CRISPR)-associated 9 nucleases (Cas9)3,8
Of these, the third system is the most promising and is receiving the most attention from researchers.
Compared to gene therapy, gene editing is still in its infancy. However, researchers from the U.S. have successfully used this method to correct the mutation of the hemoglobin gene that causes sickle cell anemia.1 Many clinical trials (large studies on patients) are testing gene editing for various diseases.
In other words, this is a rapidly developing and promising area of research. Still, gene editing is risky: accidentally editing the wrong genes could spell disaster, which is why extensive testing is necessary before gene editing becomes widely available.
What Diseases Are Candidates for Genetic Treatment?
In theory, any disease with a genetic component is a potential candidate for genetic treatment. Acne qualifies, because a family history of acne makes a person more likely to develop the disease.
However, developing, testing, and obtaining government approval for a new genetic treatment is a massive undertaking. As a first priority, scientists are focusing their research efforts on diseases that:
- Are very serious
- Have no other cure
- Result from a problem with a single gene1,2
Acne does not fit these criteria because it is not life-threatening, can improve with existing treatments, and most likely results from many factors, including multiple genes. Therefore, right now no genetic treatments for acne are available or are even far enough in development to be tested on patients.
Diseases currently treated with gene therapy

As of 2018, according to an article in The Journal of Gene Medicine, gene therapy treatments were only available for six dangerous diseases.3
However, in recent years, many more gene therapy treatments have been approved for life-threatening diseases by medical regulatory bodies in Europe and the U.S.13,14
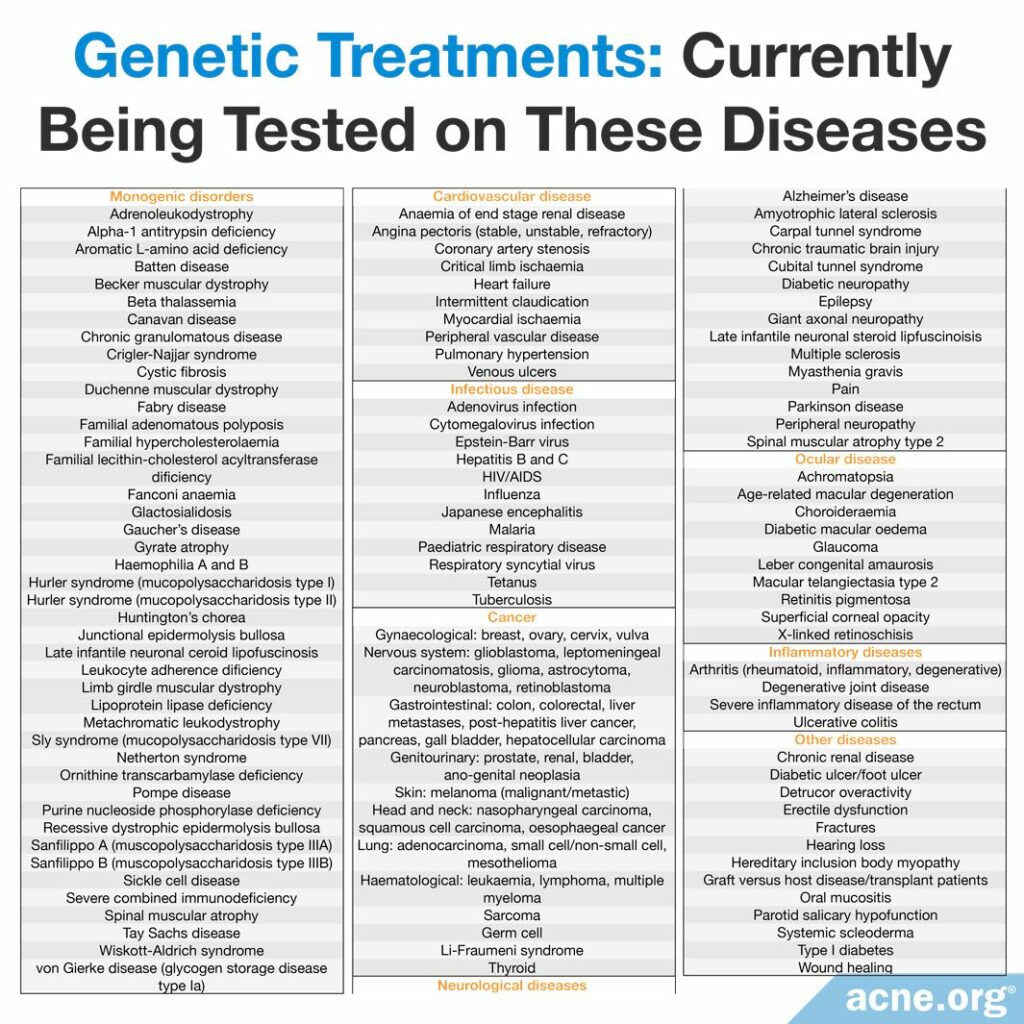
Diseases for which genetic treatments are currently being tested
In addition, clinical trials (large studies testing gene therapy on patients) are underway for many other diseases.15-18 The vast majority of these clinical trials (over 60%) are taking place in the United States.3
The table below shows the disorders for which regulatory agencies have approved clinical trials.3 As you can see, acne is not on this list. This means that right now, no clinical trials are taking place to test genetic treatments for acne.
How Safe Is Gene Therapy?

Gene therapy is relatively new and mostly still in the research phase. According to an article published in 2017 in the Brazilian scientific journal Einstein (São Paulo), “Currently, gene therapy is an area that exists predominantly in research laboratories, and its application is still experimental.”1 This means that we do not yet know how safe most genetic treatments are.
Changing or replacing genes can lead to unpredictable health risks. Previous studies have reported some cases of serious side effects of gene therapy, such as toxicity, inflammation, and even cancer.2 This is why medical and research institutions work together with regulatory agencies to ensure that people participating in clinical trials are as safe as possible. The following organizations oversee clinical trials in the United States:
- The U.S. Food and Drug Administration (FDA): The FDA approves drugs for use in clinical trials. In other words, researchers who want to test a gene therapy treatment on patients have to ask the FDA for permission.
- The National Institutes of Health (NIH): The NIH monitors clinical research and provides protocols (procedures to follow) for conducting clinical trials. In other words, researchers who want to test a gene therapy treatment on patients have to follow procedures established by the NIH.
- The NIH Recombinant DNA Advisory Committee (RAC): The RAC reviews protocols (standard procedures) for genetic treatments. In other words, researchers who want to test a gene therapy treatment on patients have to follow procedures approved by the RAC.
- The Institutional Review Board (IRB): Each hospital or university that conducts clinical trials has its own IRB, which reviews all proposed research on people to ensure the research is ethical. In other words, researchers who want to test a gene therapy treatment on patients have to obtain approval from the IRB at their hospital or university.
- The Institutional Biosafety Committee (IBC): Each hospital or university that conducts clinical trials has its own IBC. The IBC reviews all proposed research involving biological materials to ensure the research is safe for both patients and for the researchers and/or doctors. In other words, researchers who want to test a gene therapy treatment on patients have to obtain approval from the IBC at their hospital or university.1,2
Is Gene Therapy Ethical?
Some government officials and scientists question whether gene therapy is ethical (morally right).
When it comes to changing the genes in a person’s somatic cells (cells in non-reproductive organs, such as the skin, brain, or kidneys), most scientists agree that gene therapy is ethical. This is because changes in the somatic cells only affect that individual, but do not get passed on to his or her children. In other words, we are not changing the DNA of future generations of humans when we perform gene therapy on somatic cells.
On the other hand, changing the genes in a person’s germline cells (reproductive cells like a sperm or egg) is a subject of intense debate around the world. The issue is that changes in germline cells get passed on to the children of the person who receives the treatment. The idea of changing the DNA of future generations of humans makes many people nervous. In the U.S., as in many other countries, scientists cannot use government funds for germline gene therapy research. In addition, the FDA refuses to even look at proposals to test germline gene therapy on patients.1,18
The Bottom Line
While genetic treatment has become a reality for a small number of life-threatening diseases, no such treatment is yet on the horizon for acne. Intensive research into genetic treatments for many other diseases gives us reason to hope that scientists will soon develop the tools to start exploring gene therapy for acne. If and when this day comes, a genetic treatment could put a dent in acne, but is unlikely to completely eliminate it, since acne is likely caused by more than just genes.
References
- Gonçalves, G. A. R., Paiva, R. M. A. Gene therapy: advances, challenges and perspectives. Einstein (Sao Paulo), 15, 369-375 (2017). https://www.ncbi.nlm.nih.gov/pubmed/29091160
- Lister Hill National Center for Biomedical Communications. Cells and DNA. Help Me Understand Genetics (2017). https://ghr.nlm.nih.gov/primer
- Ginn, S. L., Amaya, A. K., Alexander, I. E., Edelstein, M. & Abedi, M. R. Gene therapy clinical trials worldwide to 2017: An update. J. Gene Med. 20 (5): e3015 (2018). https://www.ncbi.nlm.nih.gov/pubmed/29575374
- Melnik, B. C. FoxO1 – the key for the pathogenesis and therapy of acne? J. Dtsch Dermatol. Ges. 8, 105-114 (2010). https://pubmed.ncbi.nlm.nih.gov/20151947/
- Szabó, K. & Kemény, L. Studying the genetic predisposing factors in the pathogenesis of acne vulgaris. Hum. Immunol. 72, 766-773 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21669244
- Khan, S., Mahmood, M. S., Rahman, S. U., Zafar, H., Habibullah, S., Khan, Z. & Ahmad, A. CRISPR/Cas9: the Jedi against the dark empire of diseases. J. Biomed. Sci. 25 (1): 29 (2018). https://www.ncbi.nlm.nih.gov/pubmed/29592810
- Petridis, C., Navarini, A. A., Dand, N., Saklatvala, J. et al. Genome-wide meta-analysis implicates mediators of hair follicle development and morphogenesis in risk for severe acne. Nat. Commun. 9 (1): 5075 (2018). https://www.ncbi.nlm.nih.gov/pubmed/30542056
- Virtanen, M., Smith, S. K., Gedde-Dahl, T. Jr, Vahlquist, A. & Bowden, P. E. Splice site and deletion mutations in keratin (KRT1 and KRT10) genes: unusual phenotypic alterations in Scandinavian patients with epidermolytic hyperkeratosis. J. Invest. Dermatol., 121, 1013-20 (2003). https://www.ncbi.nlm.nih.gov/pubmed/14708600
- Gorell, E., Nguyen, N., Lane, A. & Siprashvili Z. Gene therapy for skin diseases. Cold Spring Harb. Perspect. Med. 4 (4): a015149 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24692191
- Hirsch, T. et al. Regeneration of the entire human epidermis using transgenic stem cells. Nature. 551, 327-332 (2017). https://www.ncbi.nlm.nih.gov/pubmed/29144448
- Servik, K. A boy with a rare disease gets new skin, thanks to gene-corrected stem cells. https://www.sciencemag.org/news/2017/11/boy-rare-disease-gets-new-skin-thanks-gene-corrected-stem-cells
- Bauer, J. W., Koller, J., Murauer, E. M. et al. Closure of a large chronic wound through transplantation of gene-corrected epidermal stem cells. J Invest Dermatol. 137, 778-781 (2017). https://pubmed.ncbi.nlm.nih.gov/27840234/
- Paul-Ehrlich-Institut, https://www.pei.de/EN/medicinal-products/atmp/gene-therapy-medicinal-products/gene-therapy-node.html
- Food and Drug Administration (FDA), Approved Cellular and Gene Therapy Products: https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/approved-cellular-and-gene-therapy-products
- Crudele, J. M. & Chamberlain, J. S. AAV-based gene therapies for the muscular dystrophies. Hum Mol Genet. 28, R102-R107 (2019). https://pubmed.ncbi.nlm.nih.gov/31238336/
- Nakajima, A. Application of cellular gene therapy for rheumatoid arthritis. Mod Rheumatol. 16, 269-275 (2006). https://pubmed.ncbi.nlm.nih.gov/17039306/
- Fumoto, S., Kawakami, S., Hashida, M. & Nishida, K. Targeted Gene Delivery: Importance of Administration Routes. Available at: https://www.intechopen.com/books/novel-gene-therapy-approaches/targeted-gene-delivery-importance-of-administration-routes
- Dunbar, C. E., High, K. A., Joung, J. K., Kohn, D. B., Ozawa, K. & Sadelain, M. Gene therapy comes of age. Science, 359 (6372) pii: eaan 4672 (2018). https://www.ncbi.nlm.nih.gov/pubmed/29326244
- Das, S. K., Menezes, M. E., Bhatia, S., Wang, X. Y., Emdad, L., Sarkar, D. & Fisher, P. B. Gene therapies for cancer: Strategies, challenges and successes. J. Cell. Physiol. 230, 259-71 (2015). https://www.ncbi.nlm.nih.gov/pubmed/25196387
The post Genetic Treatments for Acne appeared first on Acne.org.











