Views: 0
A Serious and Painful 2-Step Procedure for Moderate-to-severe Acne Consisting of Topical Application of a Photosensitizing Agent Followed by Shining Red and/or Blue Light on the Skin

The Essential Info
What It Is: Photodynamic therapy is a serious procedure performed in a doctor’s office that is normally reserved for moderate-to-severe cases of acne. The following two steps are undergone every 2 – 4 weeks and are repeated for a total of about 3 – 5 times over the course of a couple/few months:
- A product called a photosensitizer is applied to the skin, which makes the skin more sensitive to light.
- Powerful medical lamps with red and/or blue light are shone on the skin for about 15-20 minutes. Alternately, some doctors are now using lasers or a type of light called pulsed dye light (PDT).
Photodynamic therapy helps shrink oil glands, which in turn can reduce acne. Studies show an average of 60% reduction in acne, and results appear to last for months afterward, and perhaps long term.
What It Costs: When all is said and done, it normally costs between $1200 – $2400.
Side Effects: Most people who undergo photodynamic therapy claim that it is intensely painful, with some people claiming it is the most pain they have ever experienced in their lifetime. It also comes with far more severe side effects than traditional light therapy, including redness, swelling, itching, and peeling and/or crusting for a week or so after the procedure, as well as the potential–especially in darker-skinned people–for hyperpigmentation (skin darkening) that can last for as long as one month after the procedure. Most people choose not to leave the house for several days after undergoing photodynamic therapy.
Caution: Because photodynamic therapy impairs oil glands, and may shrink them long term, this means it can potentially permanently alter the skin, which might lead to unknown consequences such as premature aging or other unknown issues down the road. No one knows the long-term effects of photodynamic therapy, so it should be met with caution. Having said that, for people with severe acne, photodynamic therapy can present an alternative to isotretinoin (Accutane®), and may be worth a conversation with your doctor.

The Science
- How Is It Performed?
- What Type of Light Is Best?
- Which Photosensitizing Agent Is Best?
- Side Effects
- Results
- Cost
- The Bottom Line
For about a dozen years now, dermatologists have begun providing a more intense version of light therapy to their patients in a 2-step procedure which helps traditional light therapy work better by helping to shrink or destroy skin oil glands, albeit with more side effects.
Photodynamic therapy (PDT) is normally administered at 2 – 4 week intervals for a total of 3 – 5 sessions and can cost anywhere from $1200 to $2400.
It is often reserved for moderate-to-severe acne because of the seriousness of the procedure and the downtime involved.
How Is It Performed?
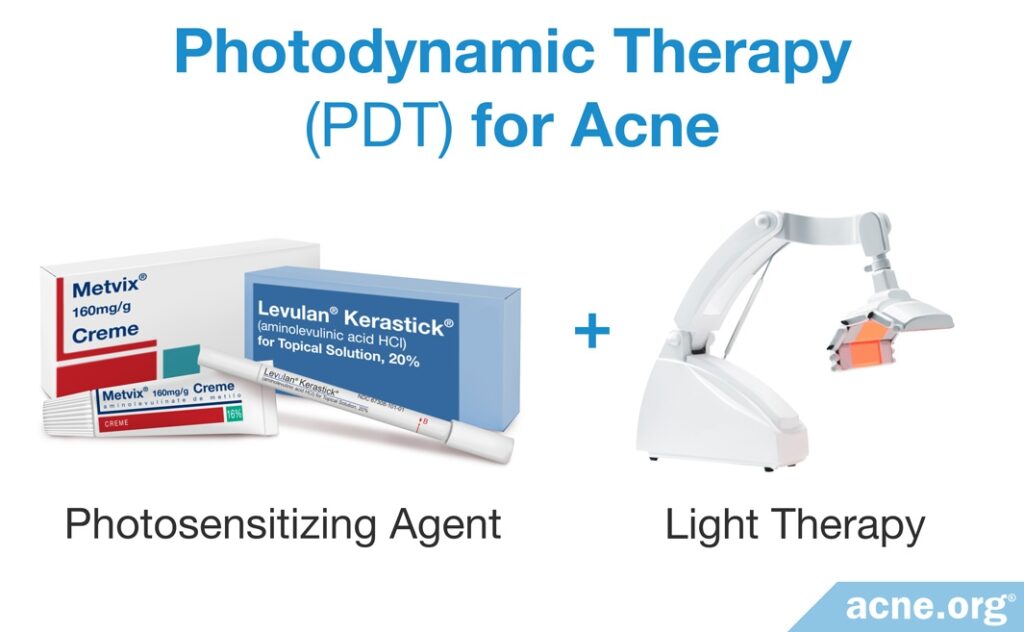
Step 1 – Photosensitizing Agent Is Applied: A photosensitizing agent is applied and allowed to absorb into the skin under an occlusive dressing for up to 3 hours. The application of a photosensitizing agent makes the skin more sensitive to light, and is what makes photodynamic therapy more intense and more effective than traditional light therapy.
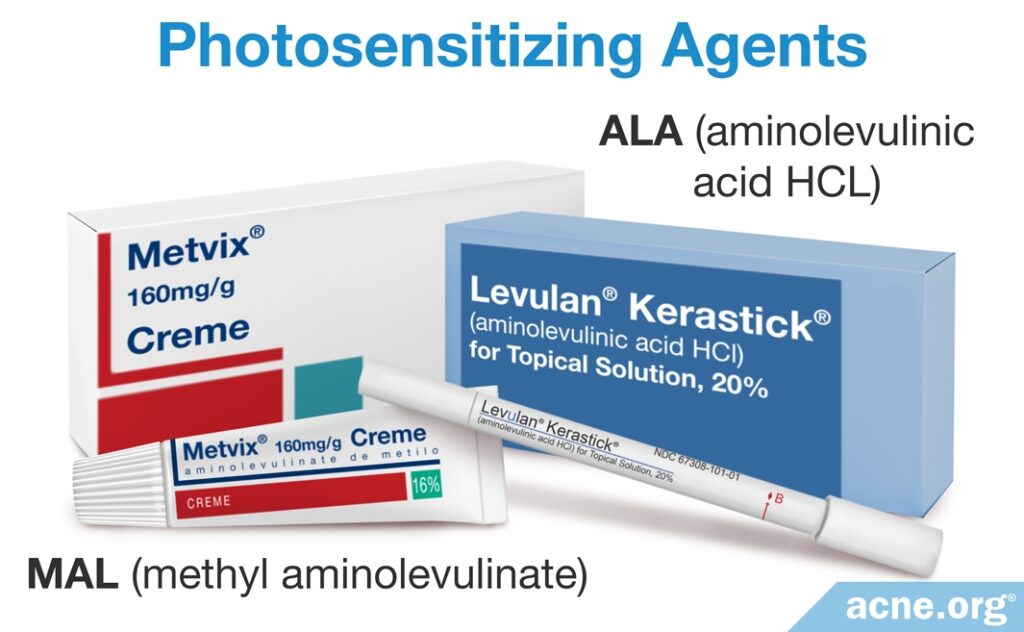
The two most commonly used photosensitizing agents are:
- 5 – 20% solution of 5-aminolevulinic acid (ALA) – often referred to by its brand name Levulan®
- 20% solution of methyl aminolevulinate (MAL)
Step 2 – The Skin Is Illuminated with Light: Professional medical lamps shine intense light on the skin, normally for 15 – 20 minutes. This light activates the photosensitizing agent, which helps shrink oil glands and also kills acne bacteria.
More recently, practitioners have begun using lasers and pulsed dye light as sources of light in PDT procedures as well.
What Type of Light Is Best?

This is a critical topic when it comes to acne and something that may account for the limited or entire lack of success some people experience with PDT.
Red and/or blue LED light are most commonly used for PDT. Research suggests that red light, because of its longer wavelength, penetrates deeper into the skin than blue light and can work better for deeper lesions.1 If your dermatologist wants to use only blue light for PDT, ask why this is the case.
Expand to read details of research

According to a 2014 review article in the journal Clinical Cosmetic and Investigational Dermatology, “Although blue light allows sufficient tissue penetration for the treatment of thin actinic keratosis (small, rough, raised areas found on areas of your skin), red light penetrates deeper and is more effective for the treatment of thicker lesions and deeper targets such as the sebaceous gland… The literature has focused primarily on MAL-PDT followed by red light because targeting of the sebaceous glands is optimized with this regimen.”1
A new device that uses a combination of red and green LED light has also recently been introduced. Although evidence for the efficacy of this device is limited, one study reported that it reduced acne by 89% and did not produce severe side effects.2 More studies will be required to adequately estimate the results of this new green light device.
Practitioners have also begun using lasers instead of LED light as sources of light in PDT procedures. The main difference between lasers and LED light devices is that lasers shine light on a smaller, more focused area of the skin, and emit stronger light to that area compared to LED devices. The advantage of using lasers is that they may require a shorter incubation time with the photosensitizer.3
Intense pulsed light (IPL) can also be used. IPL uses high-powered light sources that flash light onto the skin. Unlike LED light devices and lasers, which shine light of a specific color, IPL shines broad-spectrum light that includes wavelengths of 500 to 1200 nm.4 Intense pulsed light combined with the photosensitizer ALA seems to result in a moderate reduction (55-65%) in acne, although studies that evaluated the effectiveness of IPL have a small sample size and more studies are needed in order to reach a conclusive result.5-7
Which Photosensitizing Agent Is Best?
This is also an important topic and one that may partially account for the frustration of people who do not achieve the results they desire with PDT.
With acne in particular, methyl aminolevulinate (MAL) may be a better choice as a photosensitizing agent since it may have a higher affinity for fatty environments like skin oil glands and the skin oil therein. MAL may also achieve deeper skin penetration than 5-aminolevulinic acid (ALA).
When it comes to ALA, a higher concentration appears to be more effective at reducing acne lesions. One study found that using 10% ALA as a photosensitizing agent achieved better results than using 5% ALA. However, the researchers noted that using the higher concentration led to increased pain during the first treatment session.8
Recently, researchers have been testing a new photosensitizer with anti-inflammatory properties called indole-3-acetic acid (IAA), which has been shown to have fewer side effects than ALA or MAL, including far less pain during the procedure. However, it also produces less damage to the skin oil glands, which may result in lower efficacy. Two studies, both of which used a small sample size, reported that IAA treatment results in a more modest reduction in acne (about 30% reduction) compared to ALA treatment.9,10 However, IAA produces less pain and swelling and may therefore be a good option for those who experience severe pain or swelling with ALA or MAL treatment. IAA has not been approved for use in the United States yet, but may become available in the future.
The length of time that the physician allows the chosen photosensitizer to incubate is also important to the success of PDT. Some evidence is showing that a full 3-hour (180 minute) incubation time may be best.1 Due to crowdedness inside doctors’ offices and the desire for patient turnover, this incubation time can be cut short, potentially sacrificing results. However, if lasers or intense pulsed light are used in combination with ALA, incubation time of only 45 minutes is sufficient.3 Be sure to carefully ask your doctor about incubation time.
Side Effects
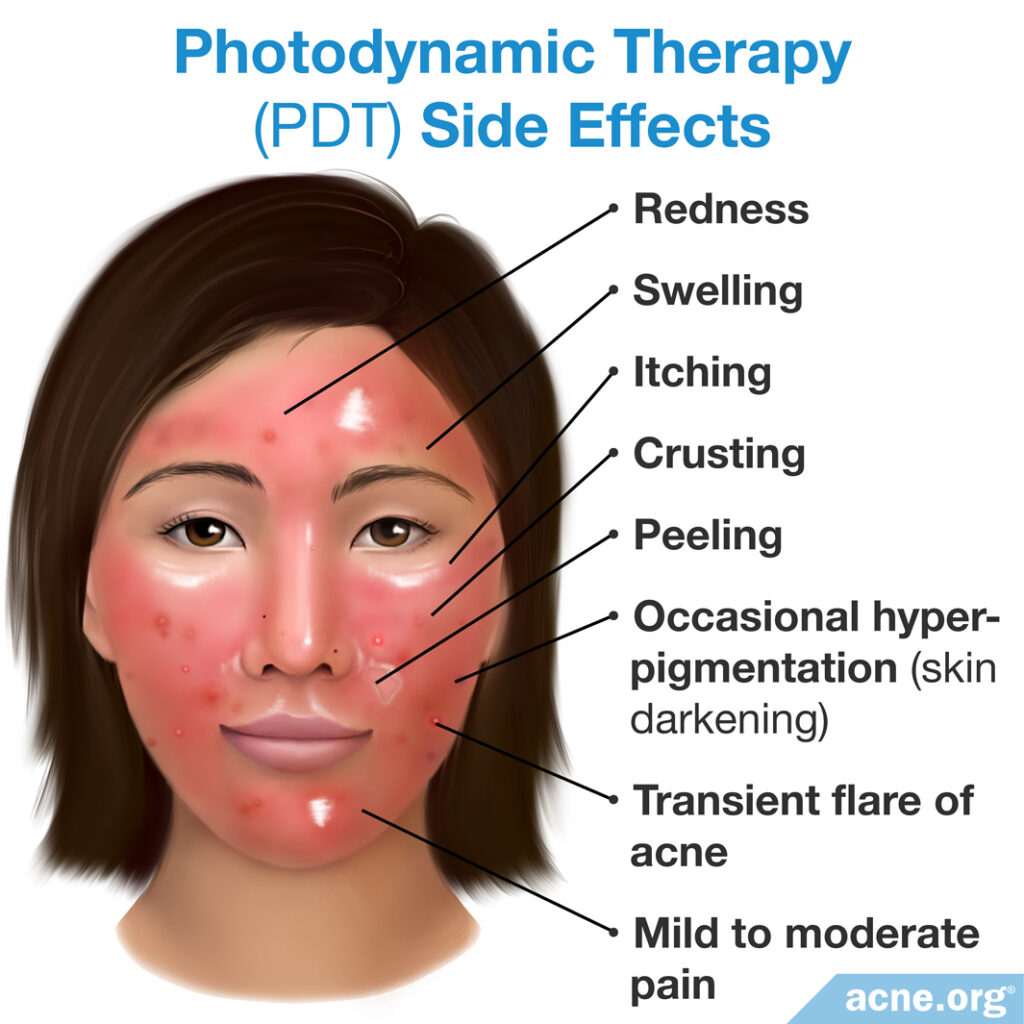
In contrast to at-home light devices without photosensitizing agents, patients undergoing photodynamic therapy in a dermatologist’s office can expect to experience pain during treatment, sometimes severe. Your doctor may be able to limit the pain by treating you with less intense light over a longer treatment session.11 This may be worth a conversation with your dermatologist prior to starting PDT.
Side effects of PDT also include redness, swelling, itching, and peeling and/or crusting for a week or so, as well as occasional hyperpigmentation (skin darkening) that can last for a month after the procedure and is more common in people of darker skin types. Most people prefer not to leave the house for several days after the procedure. Patients may also experience a flare of acne that is transient in nature and should subside. Because the skin is highly photosensitized, it is also imperative that patients stay completely out of the sun and even avoid bright indoor light for 2 days after treatment.
Side effects vary depending upon the type of photosensitizer used, with MAL tending to produce the most severe pain during treatment and potentially a higher chance of hyperpigmentation. Researchers are currently performing studies on lower concentrations of photosensitizers to gauge whether this will provide the same results with fewer side effects.4,12-14 As mentioned, researchers are also looking into other photosensitizers that produce less pain, fewer side effects, and require shorter incubation times, such as indole-3-acetic acid (IAA) with green light.10 Unlike ALA and MAL, IAA reduces the amount of skin oil without causing destruction of skin oil glands, which accounts for fewer side effects experienced with IAA compared to ALA or MAL treatment, but may also produce shorter-term results.14
Regardless of which source of light is used, most patients report feeling mild to moderate pain and swelling and peeling of the skin after photodynamic therapy.15 These side effects are temporary and usually go away 1-2 weeks after treatment.
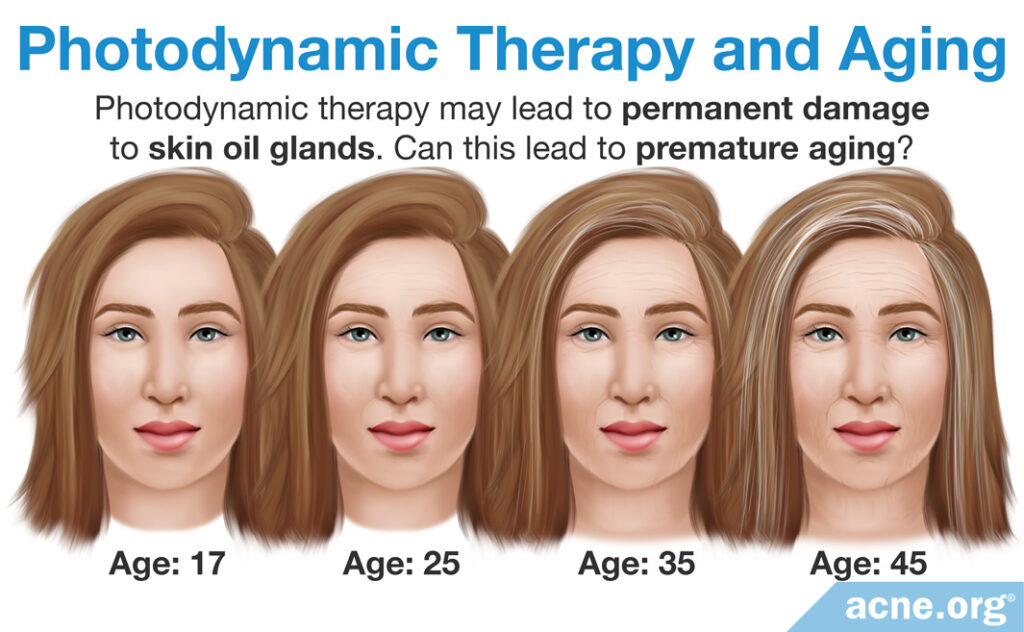
Long-term side effects: Photodynamic therapy is still a relatively new treatment and studies have not evaluated potential long-term side effects. PDT works primarily by shrinking oil glands. It shrinks them from what we can see from studies for at least 3 months and perhaps much longer or even permanently. This can be a double-edged sword. On the positive side, it can reduce acne since smaller oil glands normally lead to less acne. But on the negative side, skin oil performs several roles in human skin, including limiting bacteria, regulating the immune response in the skin, helping the skin retain moisture, and distributing antioxidants, hormones, and pheromones over the skin. It is unknown what the long-term consequences would be from permanently impairing skin oil output. Scientists also wonder if there are undiscovered roles of skin oil, for instance contributing to the graceful aging of the skin later in life.
Results
The following chart shows the studies performed on PDT as of 2018.
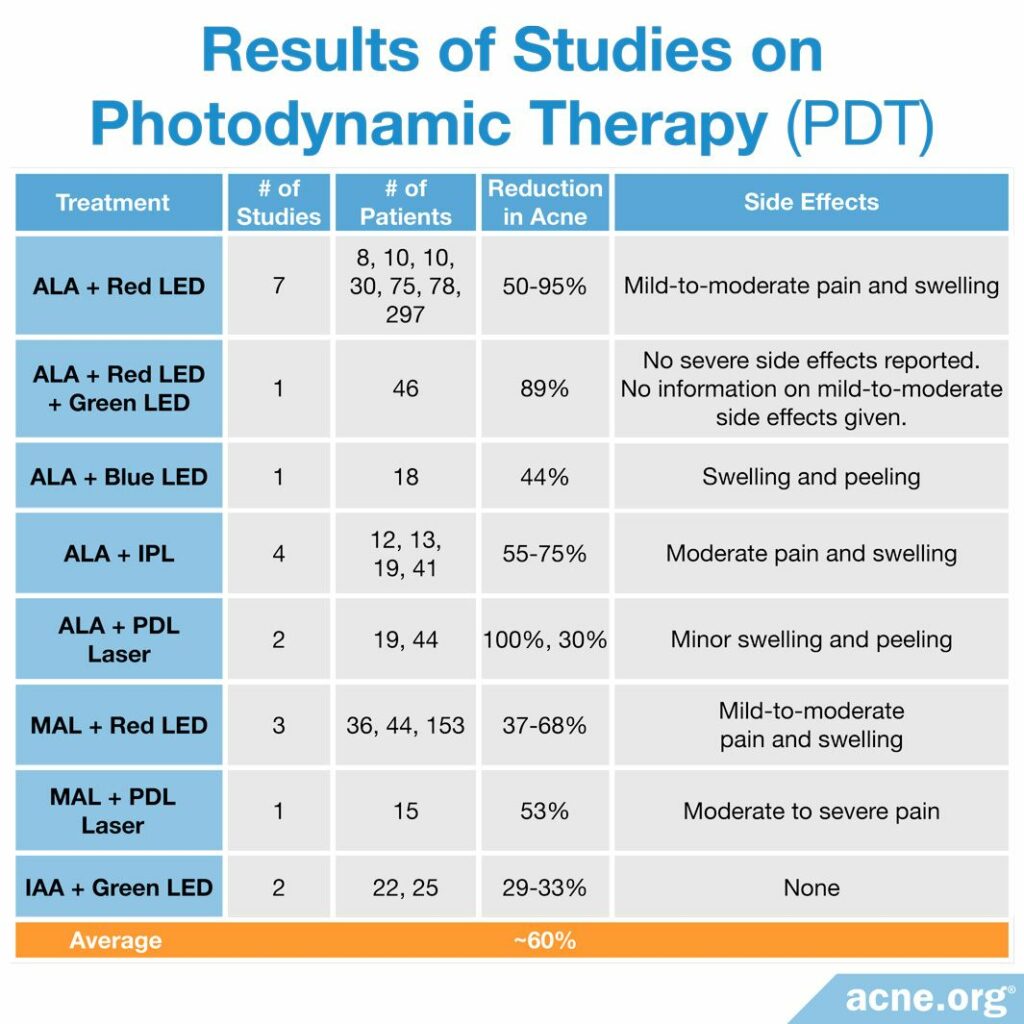
Results from studies point toward an average reduction in inflammatory acne of about 60% after 3 treatments.16,20,25,29-36 The best results are experienced by people with more severe forms of acne.2,13,21,37 When results are experienced, they tend to be semi-permanent. Researchers normally perform follow-up from studies for a maximum of 3 months, so it is hard to tell how long results last, but some dermatologists report 1- or even 2-year reduction in symptoms.
A large systematic review published in 2016 reviewed all available clinical studies that evaluated the use of photodynamic therapy. The reviewers concluded that PDT is effective, and is effective even for more severe cases of acne, and works on body acne as well.15
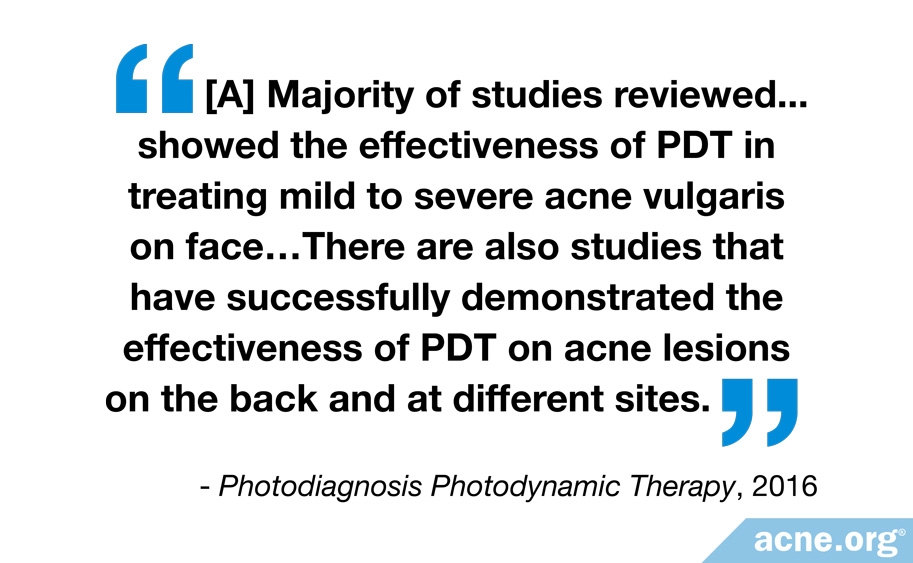
Two more recent systematic reviews agreed with this conclusion.

The first systematic review was published in the American Journal of Clinical Dermatology in 2017. The researchers combed through 69 clinical trials, 4 case reports, and 2 retrospective studies (studies that used past medical records) on PDT. They wrote, “This review supports PDT as an efficacious treatment for acne and a good adjunctive treatment for mild to severe acne, especially in patients who have not responded to topical therapy and oral antibacterials, and are not great candidates for isotretinoin.”38
The second systematic review was published in the Journal of Cosmetic Dermatology in 2020. The researchers evaluated 13 rigorous studies on PDT with a total of 701 participants and concluded that PDT is effective for treating inflammatory acne.39
However, it is important to keep in mind that while a few of the studies included large numbers of patients, most of these studies included only a small number of people and some relied on patient reports of the severity of their acne and their own satisfaction with the treatment, which is not an objective method of quantifying the results. In addition, there was a large variability in the treatments administered in each study, with researchers using different doses of photosensitizing agents (between 5 and 20% of ALA), duration of laser treatments, and treatment frequencies.15
Therefore, some reviews have held off on drawing firm overall conclusions about the efficacy of PDT for treating acne until stronger evidence, with more consistent methods, larger numbers of patients, and longer follow-up, becomes available.

For example, the authors of a review article published in the Cochrane Database of Systematic Reviews in 2016 wrote, “Due to limited evidence, we were unable to draw firm conclusions from the results of our review. In particular, the lack of long-term outcomes was a major drawback.”40

Similarly, the authors of a review article published in the British Journal of Dermatology in 2018 looked at 71 studies on PDT and noted that the quality of most studies was low. They wrote, “In summary, more robust, well-planned studies with greater sample sizes comparing the effectiveness of common acne treatments with light therapies would be welcomed.”41
Reviews on Acne.org are mixed, but keep in mind that the type of photosensitizer, incubation time, and light source used tends to vary depending on the procedure the reviewer has undergone.
Cost
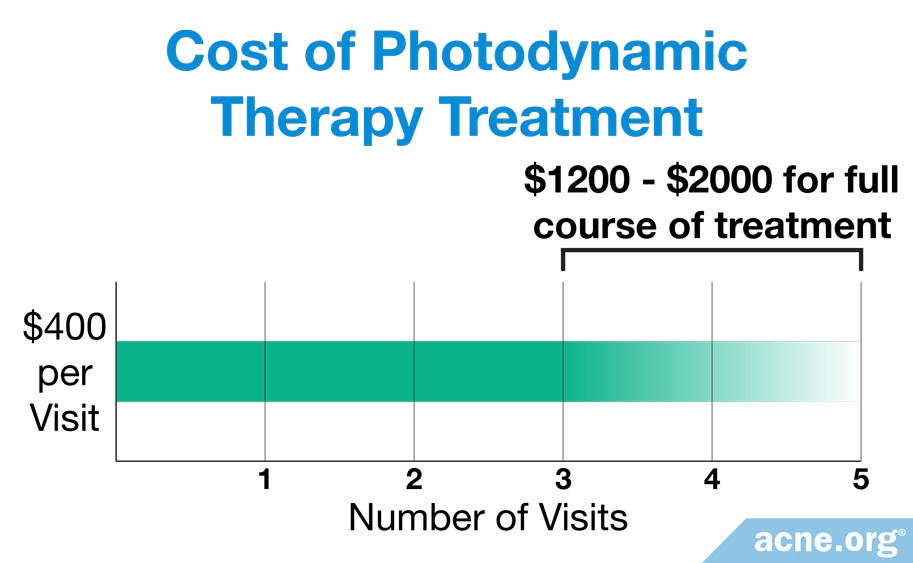
Each treatment costs on average about $400 and are normally not covered by insurance. To inquire about treatment, contact your dermatologist.
The Bottom Line
At this time, PDT looks like a promising treatment, however, we do not yet know how long the effects last, nor the long-term side effects. There are many topical treatments which can keep acne at bay which do not potentially permanently alter the skin. See a list of various acne treatments here.
References
- Wan, M. T. & Lin, J. Y. Current evidence and applications of photodynamic therapy in dermatology. Clin. Cosmet. Investig. Dermatol. 7, 145 – 163 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24899818
- Dong, Y. et al. A new LED device used for photodynamic therapy in treatment of moderate to severe acne vulgaris. Photodiagnosis Photodyn. Ther. 13, 188 – 195 (2016). https://www.ncbi.nlm.nih.gov/pubmed/26116283
- Jih, M. H. & Kimyai-Asadi, A. Laser treatment of acne vulgaris. Semin. Plast. Surg. 21, 167 – 174 (2007). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2884837/
- Bisaccia, E., Lugo, A., Johnson, B. & Scarborough, D. Intense pulsed light systems. (2006). https://en.wikipedia.org/wiki/Intense_pulsed_light
- Santos, M. A., Belo, V. G. & Santos, G. Effectiveness of photodynamic therapy with topical 5-aminolevulinic acid and intense pulsed light versus intense pulsed light alone in the treatment of acne vulgaris: comparative study. Dermatol. Surg. 31, 910 – 915 (2005). https://www.ncbi.nlm.nih.gov/pubmed/16042935
- Yeung, C. K., Shek, S. Y., Yu, C. S., Kono, T. & Chan, H. H. Liposome-encapsulated 0.5% 5-aminolevulinic acid with intense pulsed light for the treatment of inflammatory facial acne: a pilot study. Dermatol. Surg. 37, 450 – 459 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21414073
- Gold, M. H., Biron, J. A., Boring, M., Bridges, T. M. & Bradshaw, V. L. Treatment of moderate to severe inflammatory acne vulgaris: photodynamic therapy with 5-aminolevulinic acid and a novel advanced fluorescence technology pulsed light source. J. Drugs Dermatol. 6, 319 – 322 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17373194
- Zhang, J., Zhang, X., He, Y., Wu, X., Huang, J., Huang, H. & Lu, C. Photodynamic therapy for severe facial acne vulgaris with 5% 5-aminolevulinic acid vs 10% 5-aminolevulinic acid: A split-face randomized controlled study. J. Cosmet. Dermatol. 19, 368-374 (2020). https://pubmed.ncbi.nlm.nih.gov/31187937/
- Kwon, S. H. et al. A new therapeutic option for facial seborrhoeic dermatitis: indole-3-acetic acid photodynamic therapy. J. Eur. Acad. Dermatol. Venereol. 28, 94 – 99 (2014). https://www.ncbi.nlm.nih.gov/pubmed/17373194
- Huh, S. Y., Na, J. I., Huh, C. H. & Park, K. C. The effect of photodynamic therapy using indole-3-acetic Acid and green light on acne vulgaris. Ann. Dermatol. 24, 56 – 60 (2012). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3283851/
- Ibbotson, S. H., Wong, T. H., Morton, C. A., Collier, N. J., Haylett, A., McKenna, K. E., Mallipeddi, R., Moseley, H., Rhodes, L. E., Seukeran, D. C., Ward, K. A., Mohd Mustapa, M. F. & Exton, L. S. Adverse effects of topical photodynamic therapy: a consensus review and approach to management. Br. J. Dermatol. 180, 715-729 (2019). https://pubmed.ncbi.nlm.nih.gov/30183065/
- Asayama-Kosaka, S., Akilov, O. E. & Kawana, S. Photodynamic Therapy with 5% delta-Aminolevulinic Acid is Safe and Effective Treatment of Acne Vulgaris in Japanese Patients. Laser Ther. 23, 115 – 120 (2014). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4112280/
- Ma, L. et al. Low-dose topical 5-aminolevulinic acid photodynamic therapy in the treatment of different severity of acne vulgaris. Photodiagnosis Photodyn. Ther. 10, 583 – 590 (2013). https://www.ncbi.nlm.nih.gov/pubmed/24284115
- Na, J. I. et al. Indole-3-acetic acid: a potential new photosensitizer for photodynamic therapy of acne vulgaris. Lasers Surg. Med. 43, 200 – 205 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21412803
- Keyal, U., Bhatta, A. K. & Wang, X. L. Photodynamic therapy for the treatment of different severity of acne: A systematic review. Photodiagnosis Photodyn. Ther. 14, 191 – 199 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27090488
- Pollock, B. et al. Topical aminolaevulinic acid-photodynamic therapy for the treatment of acne vulgaris: a study of clinical efficacy and mechanism of action. Br. J. Dermatol. 151, 616 – 622 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15377348
- Wang, H. W. et al. Prospective study of topical 5-aminolevulinic acid photodynamic therapy for the treatment of moderate to severe acne vulgaris in Chinese patients. J. Cutan. Med. Surg. 16, 324 – 333 (2012). https://www.ncbi.nlm.nih.gov/pubmed/25772520
- Yang, G. L. et al. Short-term clinical effects of photodynamic therapy with topical 5-aminolevulinic acid for facial acne conglobata: an open, prospective, parallel-arm trial. Photodermatol. Photoimmunol. Photomed. 29, 233 – 238 (2013). https://www.ncbi.nlm.nih.gov/pubmed/24001378
- Fabbrocini, G. et al. The effect of aminolevulinic acid photodynamic therapy on microcomedones and macrocomedones. Dermatology 219, 322 – 328 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19851060
- Hong, S. B. & Lee, M. H. Topical aminolevulinic acid-photodynamic therapy for the treatment of acne vulgaris. Photodermatol. Photoimmunol. Photomed. 21, 322 – 325 (2005). https://www.ncbi.nlm.nih.gov/pubmed/16313244
- Taub, A. F. Photodynamic therapy for the treatment of acne: a pilot study. J. Drugs Dermatol. 3, S10 – 14 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15624736
- Mei, X., Shi, W. & Piao, Y. Effectiveness of photodynamic therapy with topical 5-aminolevulinic acid and intense pulsed light in Chinese acne vulgaris patients. Photodermatol. Photoimmunol. Photomed. 29, 90 – 96 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23458393
- Orringer, J. S. et al. Photodynamic therapy for acne vulgaris: a randomized, controlled, split-face clinical trial of topical aminolevulinic acid and pulsed dye laser therapy. J. Cosmet. Dermatol. 9, 28 – 34 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20367670
- Alexiades-Armenakas, M. Long-pulsed dye laser-mediated photodynamic therapy combined with topical therapy for mild to severe comedonal, inflammatory, or cystic acne. J. Drugs Dermatol. 5, 45 – 55 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16468292
- Wiegell, S. R. & Wulf, H. C. Photodynamic therapy of acne vulgaris using 5-aminolevulinic acid versus methyl aminolevulinate. J. Am. Acad. Dermatol. 54, 647 – 651 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16546587
- Bissonnette, R., Maari, C., Nigen, S., Provost, N. & Bolduc, C. Photodynamic therapy with methylaminolevulinate 80 mg/g without occlusion improves acne vulgaris. J. Drugs Dermatol. 9, 1347 – 1352 (2010). http://europepmc.org/article/med/21061756
- Pariser, D. M. et al. Photodynamic therapy with methyl aminolaevulinate 80 mg g(-1) for severe facial acne vulgaris: a randomized vehicle-controlled study. Br. J. Dermatol. 174, 770 – 777 (2016). https://www.ncbi.nlm.nih.gov/pubmed/26663215
- Haedersdal, M., Togsverd-Bo, K. & Wulf, H. C. Evidence-based review of lasers, light sources and photodynamic therapy in the treatment of acne vulgaris. J. Eur. Acad. Dermatol. Venereol. 22, 267 – 278 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18221341
- Hong, J. S., Jung, J. Y., Yoon, J. Y. & Suh, D. H. Acne treatment by methyl aminolevulinate photodynamic therapy with red light vs. intense pulsed light. Int. J. Dermatol. 52, 614 – 619 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23046014
- Hongcharu, W. et al. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J. Invest. Dermatol. 115, 183 – 192 (2000). https://www.ncbi.nlm.nih.gov/pubmed/10951234
- Wiegell, S. R. & Wulf, H. C. Photodynamic therapy of acne vulgaris using methyl aminolaevulinate: a blinded, randomized, controlled trial. Br. J. Dermatol. 154, 969 – 976 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16634903
- Akaraphanth, R., Kanjanawanitchkul, W. & Gritiyarangsan, P. Efficacy of ALA-PDT vs blue light in the treatment of acne. Photodermatol. Photoimmunol. Photomed. 23, 186 – 190 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17803597
- Goldman, M. P. & Boyce, S. M. A single-center study of aminolevulinic acid and 417 NM photodynamic therapy in the treatment of moderate to severe acne vulgaris. J. Drugs Dermatol. 2, 393 – 396 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12884461
- Horfelt, C., Funk, J., Frohm-Nilsson, M., Wiegleb Edstrom, D. & Wennberg, A. M. Topical methyl aminolaevulinate photodynamic therapy for treatment of facial acne vulgaris: results of a randomized, controlled study. Br. J. Dermatol. 155, 608 – 613 (2006). https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0781.2007.00290.x
- Pinto, C., Schafer, F., Orellana, J. J., Gonzalez, S. & Hasson, A. Efficacy of red light alone and methyl-aminolaevulinate-photodynamic therapy for the treatment of mild and moderate facial acne. Indian J. Dermatol. Venereol. Leprol. 79, 77 – 82 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23254733
- Shaaban, D., Abdel-Samad, Z. & El-Khalawany, M. Photodynamic therapy with intralesional 5-aminolevulinic acid and intense pulsed light versus intense pulsed light alone in the treatment of acne vulgaris: a comparative study. Dermatol. Ther. 25, 86 – 91 (2012). https://www.ncbi.nlm.nih.gov/pubmed/22591502
- Gold, M. H. et al. The use of a novel intense pulsed light and heat source and ALA-PDT in the treatment of moderate to severe inflammatory acne vulgaris. J. Drugs Dermatol. 3, S15 – 19 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15624737
- Boen, M., Brownell, J., Patel, P. & Tsoukas, M. M. The role of photodynamic therapy in acne: An evidence-based review. Am. J. Clin. Dermatol. 18, 311 – 321 (2017). https://pubmed.ncbi.nlm.nih.gov/28276005/
- Tang, X., Li, C., Ge, S., Chen, Z. & Lu, L. Efficacy of photodynamic therapy for the treatment of inflammatory acne vulgaris: A systematic review and meta-analysis. J. Cosmet. Dermatol. 19, 10 – 21 (2020). https://pubmed.ncbi.nlm.nih.gov/31654468/
- Barbaric, J., Abbott, R., Posadzki, P. et al. Light therapies for acne. Cochrane Database Syst. Rev. 9, CD007917 (2016). https://pubmed.ncbi.nlm.nih.gov/27670126/
- Barbaric, J., Abbott, R. Posadzki, P. et al. Light therapies for acne: abridged Cochrane systematic review including GRADE assessments. Br. J. Dermatol. 178, 61 – 75 (2018). https://pubmed.ncbi.nlm.nih.gov/28338214/
The post Photodynamic Therapy – PDT appeared first on Acne.org.

