Views: 0
This Depends on How Much Vitamin D You Already Have in the Blood, but 4000 IU (100 mcg) or More per Day Is Likely to Be Dangerous

The Essential Info
Vitamin D is a crucially important nutrient that the skin produces during exposure to sunlight, but which can also be obtained through supplementing with oral Vitamin D.
Some emerging evidence suggests that it might play a role in preventing acne, and this makes sense because vitamin D is known to:
- Reduce Inflammation – acne is an inflammatory disease
- Keep Bacteria in Check – acne is in part a bacterial disease
- Promote Wound Healing – medically speaking, acne lesions are small wounds
A healthy amount of vitamin D in the blood is 30 – 50 ng/mL, and only people whose vitamin D levels fall below this range should take supplements. You can ask your doctor for a routine and simple blood test to determine your level. If your levels are low, your doctor will recommend the amount of vitamin D for you to supplement.
How Much Is Too Much? The Institute of Medicine considers more than 4000 IU (100 mcg) per day to be dangerous because vitamin D is fat-soluble, which means it can build up in the body’s fat cells and become toxic. Taking too much vitamin D can cause serious side effects, such as:
- Weak bones
- Kidney stones
- Problems with heart and brain function
The Bottom Line: It’s worth it to get your vitamin D level checked. Vitamin D is critically important to the health of the body and the skin and many people are deficient. If your doctor finds that you are deficient, follow his or her supplementation recommendations, and don’t overdo it. Make sure to get your blood rechecked and monitor your progress so your levels don’t get too high.
My Experience: When I started researching vitamin D and acne, I got my blood level of vitamin D checked. It came back at around 22 ng/mL, which is considered low. My doctor told me to take 4000 IU per day and come back and see him in a couple of months. I didn’t listen, and instead decided to buy a 10,000 IU supplement. I kept taking that much every day and went back to the doctor and got another vitamin D test. My level was 105 ng/mL, which put me at risk for toxicity. My doctor scolded me to stop taking the supplement immediately. Take it from me, don’t over-supplement!

The Science
- Vitamin D and Acne
- Where Do We Get Vitamin D?
- How Much Vitamin D Should We Have in the Blood?
- In Summary
Vitamin D and Acne
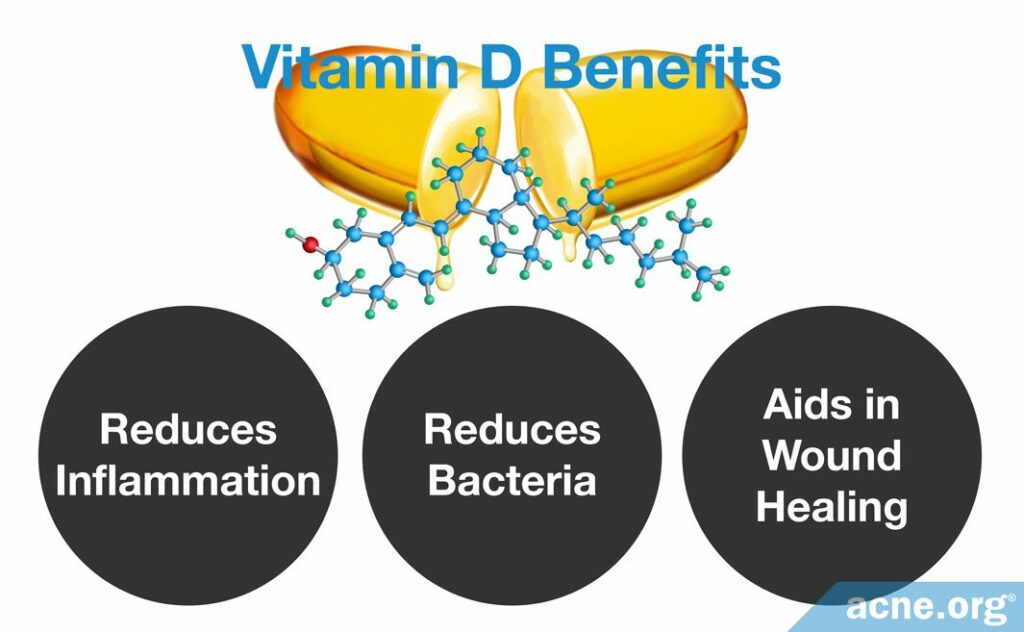
Vitamin D is an important nutrient that helps our bodies with multiple crucial functions1,2, several of which are relevant to acne, including:
- Reducing Inflammation: Inflammation is one of the first steps in the development of acne lesions, and is present throughout an acne lesion’s entire life cycle.
- Reducing bacteria: A strain of bacteria called Cutibacterium acnes (C. acnes) leads to some of the redness and pain in and around acne lesions.
- Aiding wound healing: Acne lesions themselves are a small type of wound.
Research has already shown that vitamin D can help in treating other skin conditions, such as psoriasis and atopic dermatitis.1,3 However, we currently only have a small amount of mostly indirect evidence that vitamin D helps with acne. Five studies have found that people with acne, especially severe acne, tend to be deficient in vitamin D.3-7 Two of these studies also found that giving vitamin D supplements to people with acne who are vitamin D-deficient improves their acne.4,7
Expand to read details of these 5 studies
A study published in the journal Dermato-Endocrinology in 2014 looked at the amount of vitamin D in the blood of people with nodulocystic (severe) acne compared to people without acne. The researchers found that people with nodulocystic acne had lower levels of vitamin D in their blood. The authors of the study wrote, “The patients with nodulocystic acne had relatively low [blood] vitamin D levels compared with the subjects in the control group.”3

Another study, published in the journal PLoS ONE in 2016, also found a connection between blood vitamin D levels and acne. The researchers measured vitamin D levels in 80 people with acne and 80 people without acne. The scientists found that 48.8%, or almost half, of people with acne were deficient in vitamin D, compared to only 22.5%, or less than a quarter, of people without acne. The researchers also noticed that people with more severe acne tended to have lower vitamin D levels compared to people with milder acne.
To test the idea that correcting a vitamin D deficiency might help with acne, the researchers gave the vitamin D-deficient people with acne a vitamin D3 supplement at 1000 IU/day for 2 months. All patients who received the vitamin D supplement experienced an improvement in acne lesions. However, the researchers noted, “A further study with a larger sample size is needed to confirm our results because of the small number of patients in the supplementation study and the natural fluctuation of acne.”4
A study published in the Journal of Cosmetic Dermatology in 2019 also found that vitamin D deficiency tends to go hand-in-hand with acne. The researchers tested 90 people with acne and 60 people without acne for vitamin D deficiency. They found significantly lower blood levels of vitamin D in the people with acne.5
Curiously, the scientists found that treating acne with isotretinoin (an oral medication that doctors sometimes prescribe for severe acne) not only improved acne, but also improved vitamin D levels. This led them to wonder whether acne itself decreases vitamin D levels by reducing the skin’s ability to produce vitamin D during sun exposure.5 In other words, the relationship between vitamin D levels and acne might be a two-way street: vitamin D deficiency might contribute to acne, and acne might contribute to vitamin D deficiency. However, more research is needed before we can be sure exactly how acne and vitamin D are related.
A study published in the Journal of Cosmetic Dermatology in 2021 combed through 13 articles comparing vitamin D levels in people with and without acne. The 13 studies included a total of 918 people with acne and 814 people without acne. After analyzing all the data from these studies, the researchers concluded that people with acne have lower levels of vitamin D on average compared to people without acne. In addition, people with acne are more likely than people without acne to have a low enough level of vitamin D to be considered a deficiency.6

Similarly, a study published in the Journal of Dermatological Treatment in 2019 compared vitamin D levels between 100 people with acne and 100 people without acne. The scientists found that 34% of people with acne were deficient in vitamin D, compared to only 12% of people without acne.
Next, the researchers tested the idea that taking an oral vitamin D supplement might help with acne. They randomly divided the people with acne into two groups:
- Group 1 received a daily oral supplement containing an active form of vitamin D called alfacalcidol, which is more potent than over-the-counter vitamin D.
- Group 2 received a daily placebo (a similar-looking oral supplement without vitamin D).
The experiment continued for 3 months. At the end of the experiment, the people in Group A had higher vitamin D levels than the people in Group B. In addition, after taking the vitamin D supplement for 3 months, the people in Group A had lower inflammation and significantly improved acne compared to the start of the experiment.7
These findings suggest that having less vitamin D in the blood makes a person more likely to develop severe acne. However, we need to keep one point in mind: the studies do not show a cause-and-effect relationship. In other words, they do not demonstrate that if a healthy person becomes vitamin D-deficient, he or she will develop severe acne. Therefore, as is often the case with emerging scientific research, we must exercise caution when examining the results.
Still, it may be prudent for anyone with acne, and especially those with severe acne, to ask their doctor to order a blood test to see if they are deficient in vitamin D. The test for vitamin D deficiency is an easy blood test, and anyone can ask for one.
Doctors consider a blood vitamin D level of 30 – 50 ng/mL to be healthy. If the test shows that the level of vitamin D is below this range, a doctor may recommend supplements. It is important to follow the doctor’s instructions and not to exceed the recommended amount of supplement, since too much vitamin D can be dangerous. For daily supplements, a dose of 4000 IU (100 mcg) or more per day may be toxic.
Where Do We Get Vitamin D?
Sun exposure – does not lead to toxic levels of vitamin D
Our skin is designed to produce almost all of the vitamin D our bodies need. Whenever the sun shines on the skin, the skin synthesizes vitamin D from the cholesterol in our bodies. Our ancestors easily got all the vitamin D they needed from sun exposure. However, in today’s world, we get far less direct sun exposure, which can leave many people vitamin D-deficient.
Expand to read about how the factors that determine how much sun we need
- Skin pigmentation: The darker the skin, the more time in the sun we need to make enough vitamin D. Because each individual has a unique skin tone, each person needs a different amount of time in the sun to produce enough vitamin D.

A 2006 article in the Bulletin of the World Health Organization gave this example: “With the amount of sun that would require 10 – 12 minutes of exposure in a fair skinned person to achieve maximum vitamin D levels, it may take three times longer for an Asian Indian and up to ten times as long in a deeply pigmented African American.”8
- Amount of exposed skin: The more skin that is exposed, the less time in the sun we need for adequate vitamin D levels.8 The amount of exposed skin depends on individual clothing preferences and on weather conditions. One of the reasons that people need more time outside in the winter is that winter clothing usually covers most of the skin.
- Intensity of ultraviolet (UV) rays: The more intense the UV rays, the less time in the sun we need to make enough vitamin D. The intensity of UV rays changes depending on the geographical location and the season. Therefore, the same person may need only a few minutes of sunlight in the summer, but several hours in the winter.8,9
- Sunscreen: Sunscreen absorbs, reflects, and/or scatters UV rays before they reach the skin, which prevents the skin from using UV rays to make vitamin D.
Each of these factors can vary significantly from person to person, so it is difficult to give general recommendations for how much sun exposure the average person needs to have enough vitamin D. In general, people with the lightest skin need about 20 minutes of unprotected sun exposure per day on large areas of the body, and people with darkest skin need 2 hours or more.

It is impossible to get too much vitamin D from sun exposure. As soon as the body has made enough vitamin D from the sun it will stop.
However, it’s a different story when it comes to supplements. Since vitamin D is fat-soluble, the body stores any unused amounts of the vitamin in fat cells. This means that if you keep taking supplements, your body will keep building up its stores of vitamin D to potentially toxic levels.
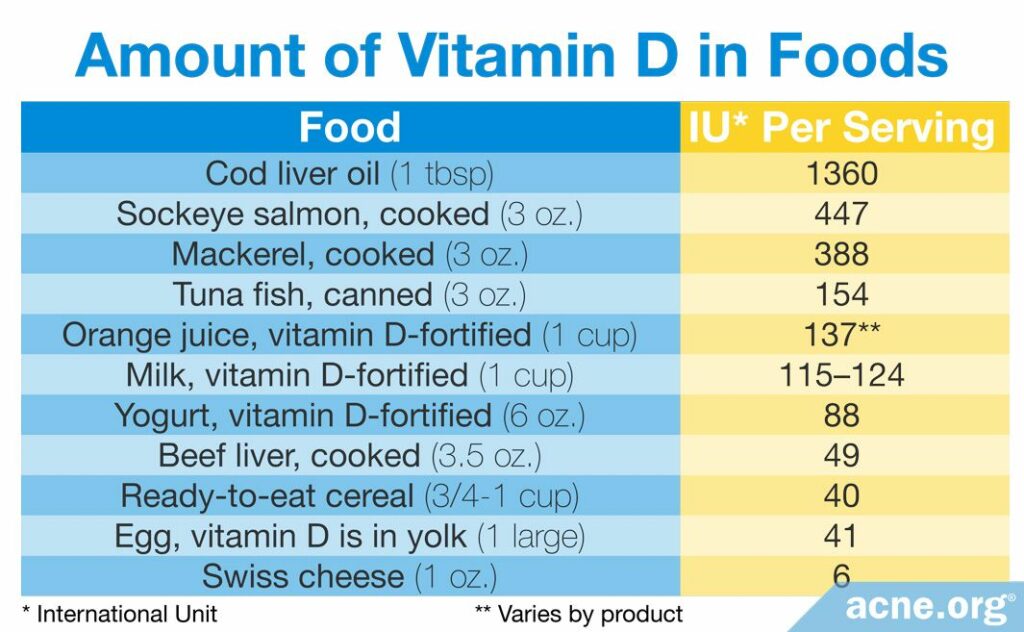
Food sources – very unlikely to lead to toxic levels of vitamin D
We can obtain a small amount of vitamin D from natural food sources by maintaining a healthy and varied diet. Vitamin D is mostly found in animal products, such as meat, fish, and eggs. Additionally, manufacturers can add vitamin D to some products, such as milk, orange juice, or cereal, to make them vitamin D – fortified.10 Unless you are taking a lot of cod liver oil or other types of fish oil, you are unlikely to reach toxic levels of vitamin D through food alone.
Vitamin D supplements – can lead to toxic levels of vitamin D
If your doctor tests your blood for vitamin D and finds that you have a vitamin D deficiency, he will probably recommend a supplement. Doctors normally do not recommend sunbathing to increase vitamin D, since it is difficult to determine how much sun exposure a particular person will need, and since too much time in the sun poses other health risks such as skin cancer.
Most people take one of these two types of vitamin D supplements:
- Vitamin D3 supplements: Most over-the-counter vitamin D, such as in multivitamins, is of this kind. Vitamin D3 is the type of vitamin D that our bodies make and that food sources normally contain. It is more bioactive, which means it is more powerful inside the body.
- Vitamin D2 supplements: Most prescription vitamin D supplements are of this kind. Vitamin D2 is made by mushrooms and fungi, as well as in commercial labs. It is the slightly less bioactive type of vitamin D.10
Some people may choose to take cod liver oil or fish oil capsules, since these contain high concentrations of vitamin D.
Regardless of which supplement you take, make sure to follow your doctor’s orders.
How Much Vitamin D Should We Have in the Blood?
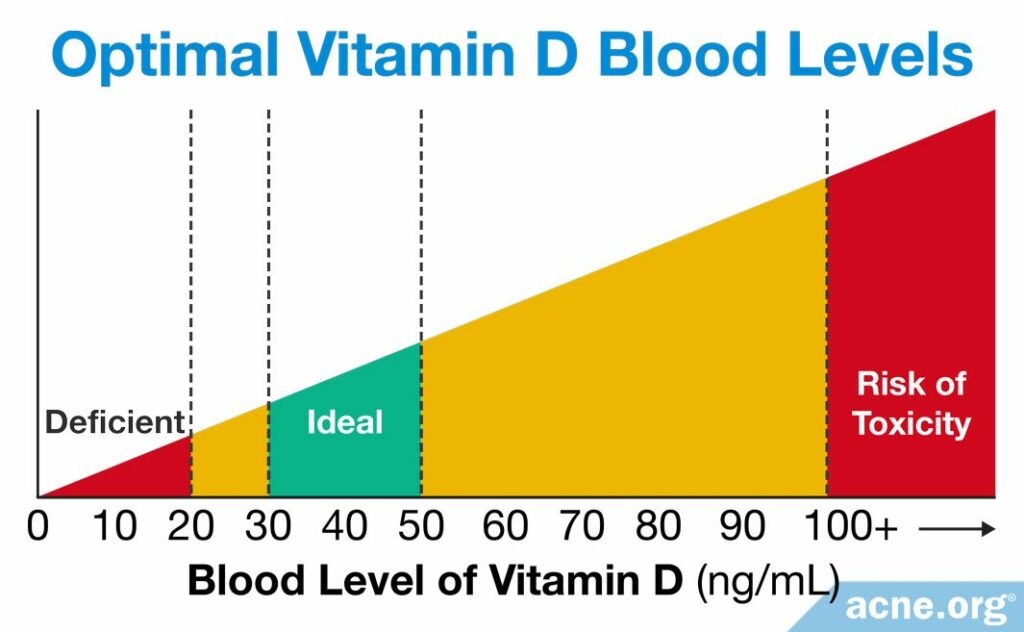
Doctors measure the concentration of vitamin D in the blood in ng/mL (nanograms per milliliter) or in nmol/L (nanomoles per liter). No matter how much time you spend in the sun, your skin will only make enough vitamin D to reach a blood level of, at most, 80 ng/mL. When your body approaches this level, it stops the production of vitamin D.
There are three main authorities that provide guidelines on how much vitamin D in the blood is safe: the Institute of Medicine, the Endocrine Society, and the Vitamin D Council. The table below summarizes their recommendations.11-13
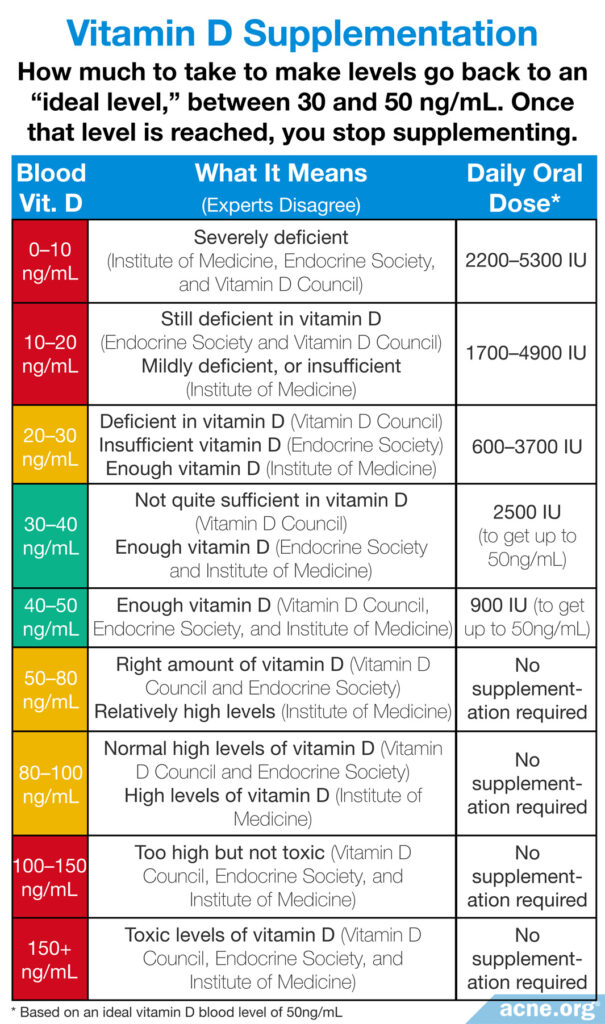
If your blood tests comes back as deficient in vitamin D, the amount you should supplement depends on the current level of vitamin D in the blood. This is why it is critical to see a doctor and undergo a blood test for vitamin D deficiency before taking any supplements. Having too little or too much vitamin D is associated with health risks.14,15
If the amount of vitamin D in the blood reaches toxic levels, several severe health problems can result. The most common one is hypercalcaemia, which means too much calcium in the blood. This happens because vitamin D is responsible for calcium absorption in the body. In other words, if we have too much vitamin D in our blood, we also will get too much calcium in the blood. Too much calcium in the blood can lead to weak bones and kidney stones, as well as heart and brain problems. Other symptoms of excess vitamin D include dehydration, vomiting, decreased appetite, irritability, constipation, fatigue, and muscle weakness.
How much vitamin D is too much?
Because the effects of taking vitamin D supplements depend on how much vitamin D is already in the blood, it is difficult to give a single answer for how much is too much.
According to the Institute of Medicine, a daily intake of 4000 IU (100 mcg) of vitamin D on an ongoing basis is harmful for the health of anyone over the age of eight.
However, there are case reports of side effects in people taking even less than 4000 IU.12
Large dosages: Your doctor may prescribe a large dosage, such as 50,000 IU, to be taken just once per month. Your body will store most of this large amount of vitamin in your fat cells, where the body can access it later as necessary. This allows you to maintain a healthy supply for days when you do not get enough sun.
Because vitamin D is fat-soluble, it is a good idea to take vitamin D supplements with moderately-fatty food, such as peanut butter, eggs, avocados, etc. Otherwise, your body may not absorb the vitamin properly.
Several studies have investigated the health risks of too much vitamin D.
Expand to read three studies on the health risks of taking too much vitamin D

One study, published in the Journal of Clinical Endocrinology & Metabolism in 2013, found that people who have less than 18 ng/mL or more than 50 ng/mL of vitamin D in the blood die sooner than people who have between 18 and 50 ng/mL. In other words, people who have too much or too little vitamin D in the blood tend to die sooner than people who have the recommended amount.14

Another large study of 420,000 patients, which was also published in the Journal of Clinical Endocrinology & Metabolism in 2013, found that people with vitamin D levels above 36 ng/mL were at higher risk for heart attack and death.14

A third large study of 247,574 patients, published in the Journal of Clinical Endocrinology & Metabolism in 2012, showed that people with vitamin D levels above 56 ng/mL were at higher risk for death.14
These three studies suggest that a blood vitamin D level above 50 ng/mL is harmful, since it can potentially lead to heart problems and earlier death. However, we must keep in mind that these studies are correlational–in other words, they cannot prove that vitamin D is what caused the health problems. To prove this, researchers would need to conduct a clinical trial. Still, from the data we currently have, it seems safe to keep your level of vitamin D between 30 and 50 ng/mL.
In addition to the three studies above, a case study published in the Journal of Pediatric Endocrinology and Metabolism in 2014 demonstrated some effects of taking too much vitamin D. The report described a 12-year-old boy who had been taking six vitamin D supplements per day for one month. This dose was equivalent to 50,000 IU/day, which is much higher than the recommended daily amount. The boy was admitted to the hospital with abdominal pain, constipation, and vomiting. Laboratory tests revealed high levels of vitamin D, kidney failure, and high blood pressure.16 The authors wrote, “[This] case report underlines that self-medication with [over-the-counter] preparations can lead to the risk of organ dysfunction and even death. They must be prescribed only when needed and under strict medical control.“16
Another case study published in the journal Endocrine, Metabolic & Immune Disorders – Drug Targets in 2021 described the effects of vitamin D overdose in an adult. In this case, a 56-year-old woman had been taking 130,000 IU of vitamin D per day for over a year and a half as part of an unconventional treatment for multiple sclerosis. The woman was admitted to the hospital with nausea, vomiting, and muscle weakness that had lasted 3 weeks. Her blood tests showed a very high level of vitamin D and calcium, and she was experiencing kidney failure. After the woman stopped taking vitamin D, her calcium levels returned to normal in one week. However, it took 6 months for her kidney function to normalize and 18 months for her blood vitamin D to return to healthy levels.17 This case demonstrates the dangers of vitamin D overdose.
In Summary
Vitamin D is an important vitamin that may help to improve acne. Our bodies make vitamin D in the skin and obtain it from food or dietary supplements. While vitamin D deficiency poses health risks, taking too much vitamin D can cause severe and possibly fatal side effects. If you think you may have a vitamin D deficiency, see your doctor and request a blood test for vitamin D levels before taking any supplements. Ideally, the amount of vitamin D in the blood should be between 30 and 50 ng/mL, and it is important not to exceed this level.
References
- Reichrath, J. Vitamin D and the skin: an ancient friend, revisited. Exp Dermatol 16, 618 – 625 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17576242
- Kamen, D. L. & Tangpricha, V. Vitamin D and molecular actions on the immune system: modulation of innate and autoimmunity. J Mol Med 88, 441 – 450 (2010). https://www.ncbi.nlm.nih.gov/pubmed/20119827
- Yildizgören, M. T. & Togral, A. K. Preliminary evidence for vitamin D deficiency in nodulocystic acne. Dermatoendocrinol 6, e983687 (2014). https://www.ncbi.nlm.nih.gov/pubmed/26413187
- Lim, S. K., Ha, J. M., Lee, Y. H., Lee, Y., Seo, Y. J., Kim, C. D., Lee, J. H. & Im. M. Comparison of vitamin D levels in patients with and without acne: A case-control study combined with a randomized controlled trial. PLoS One 11, e0161162 (2016). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4999291/
- El-Hamd, M. A., El Taieb, M. A., Ibrahim, H. M. & Aly, S. S. Vitamin D levels in acne vulgaris patients treated with oral isotretinoin. J Cosmet Dermatol 18, 6-20 (2019). https://www.ncbi.nlm.nih.gov/pubmed/29460332
- Wang, M., Zhou, Y. & Yan, Y. Vitamin D status and efficacy of vitamin D supplementation in acne patients: A systematic review and meta-analysis. J Cosmet Dermatol 20, 3802-3807 (2021). https://pubmed.ncbi.nlm.nih.gov/33690970/
- Ahmed Mohamed, A., Salah Ahmed, E. M., Abdel-Aziz, R. T. A., Eldeeb Abdallah, H. H., El-Hanafi, H., Hussein, G., Abbassi, M. M. & El Borolossy, R. The impact of active vitamin D administration on the clinical outcomes of acne vulgaris. J Dermatolog Treat 32, 756-761 (2021). https://pubmed.ncbi.nlm.nih.gov/31868550/
- Lucas, R. M., Repacholi, M. H. & McMichael, A. J. Is the current public health message on UV exposure correct? Bull World Health Organ 84, 485 – 491 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16799733
- Cancer Council Australia. Risks and benefits of sun exposure. (2007). https://www.cancer.org.au/policy-and-advocacy/position-statements/sun-smart/
- Vanchinathan, V. & Lim, H. W. A dermatologist’s perspective on vitamin D. Mayo Clin Proc 87, 372 – 380 (2012). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3498088/
- Ross, A. C., Taylor, C. L., Yaktine, A. L. & Del Valle, H. B. Dietary reference intakes for calcium and Vitamin D. National Academy of Sciences (2010). https://www.ncbi.nlm.nih.gov/books/NBK56070/
- Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 96, 1911 – 1930 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21646368
- Heaney, R. P. Assessing vitamin D status. Curr Opin Clin Nutr Metab Care 14, 440 – 444 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21832900
- Korgavkar, K., Xiong, M. & Weinstock, M. A. Review: Higher vitamin D status and supplementation may be associated with risks. Eur J Dermatol 24, 428 – 434 (2014). https://link.springer.com/article/10.1684/ejd.2014.2318
- Bouillon, R. et al. Optimal vitamin D status: A critical analysis on the basis of evidence-based medicine. J Clin Endocrinol Metab 98, 1283 – 1304 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23922354
- Conti, G. et al. Vitamin D intoxication in two brothers: Be careful with dietary supplements. J Pediatr Endocrinol Metab 27, 763 – 767 (2014). https://www.ncbi.nlm.nih.gov/pubmed/24670344
- De Vincentis, S., Russo, A., Milazzo, M., Lonardo, A., De Santis, M. C., Rochira, V., Simoni, M. & Madeo, B. How much vitamin D is too much? A case report and review of the literature. Endocr Metab Immune Disord Drug Targets 21, 1653-1659 (2021). https://pubmed.ncbi.nlm.nih.gov/33030138/
The post Oral Vitamin D: How Much Is Too Much? appeared first on Acne.org.

