Views: 0
Applying Hydrocortisone to the Skin Is More Likely to Trigger or Worsen Acne than to Reduce It

The Essential Info
Hydrocortisone is a popular steroid medication for the skin. Because hydrocortisone is available over-the-counter and can temporarily relieve redness and discomfort, many people with acne apply it to their skin in hopes of reducing breakouts.
To date, only one study has directly looked at whether hydrocortisone improves or worsens acne and showed that it has no impact. Additionally, strong evidence suggests that applying hydrocortisone to the skin on a long-term basis would make acne worse because steroids like hydrocortisone:
- Increase the growth of acne bacteria in the skin, which is likely to intensify acne.
- Increase the production of skin oil, which is likely to clog pores and worsen acne.
- Slow down the healing of wounds, which is likely to hinder healing of acne lesions.
Applying hydrocortisone on a long-term basis may also cause serious unwanted side effects such as:
- Worsening of acne
- Unwanted growth of body hair
- Darkening or lightening of the skin
- Skin infections
- Contact dermatitis (skin rash)
- Rosacea
- More systemic side effects like weight gain, impaired wound healing, irregular menstruation, changes in sexual function, and muscle weakness
The Bottom Line: Avoid
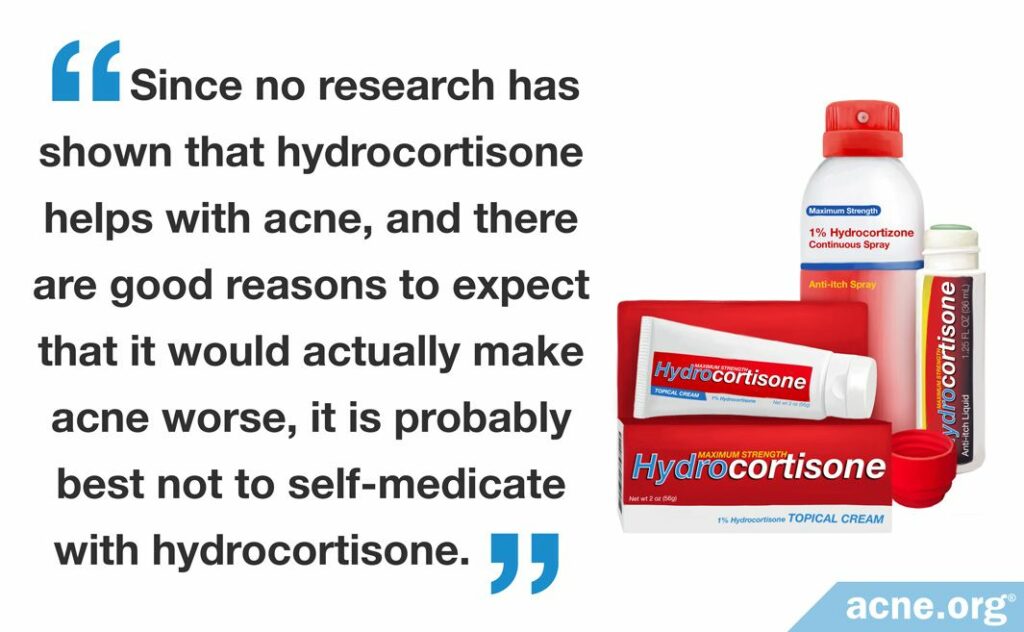
Since there are good reasons to expect that hydrocortisone will make acne worse and it can cause unwanted side effects, it is best to avoid topical hydrocortisone as an acne treatment.

The Science
- What Is Hydrocortisone?
- Hydrocortisone and Acne
- Side Effects of Topical Hydrocortisone
- The Bottom Line
Many people keep some hydrocortisone in their medicine cabinet to relieve itchy insect bites. Doctors also frequently prescribe it for skin rashes, eczema, dermatitis, and skin allergies. Since acne shares some symptoms with these conditions, like skin redness and itching, you may be tempted to try hydrocortisone on your breakouts in hopes of seeing improvement. However, the available evidence suggests that in the long run, hydrocortisone will most likely worsen your acne.
What Is Hydrocortisone?

Hydrocortisone is a hormone that the body naturally produces in the adrenal glands (hormone glands that sit on top of the kidneys) to control inflammation when we get injured or sick.
Hydrocortisone can also be artificially manufactured as a topical medication for reducing inflammation and is available at drugstores without a prescription at 1% concentration.1
Chemically speaking, hydrocortisone is a steroid. The word “steroid” may make you think of anabolic steroids that some people take in order to “bulk up,” but steroids are actually a large class of chemicals that play many different roles in the body.
All about steroids
Steroids include:
- Medications for treating inflammation: For example, hydrocortisone and dexamethasone
- Vitamin D and its derivatives: For example, vitamin D2 and vitamin D3
- Sex hormones: For example, testosterone and estrogen
- Anabolic steroids: For example, methandienone and testosterone propionate
Chemically, all steroids are related because they all possess a 4-ring carbon structure in the center.
Hydrocortisone serves as the backbone from which manufacturers produce all the other steroids that function as topical medications, such as beclomethasone.1
Medical uses of hydrocortisone
As a topical medication, hydrocortisone performs two main functions:
- Prevents or reduces inflammation (anti-inflammatory effect): Hydrocortisone blocks inflammatory processes in the skin like redness, swelling, itching, and discomfort.
- Suppresses the body’s immune response (immunosuppressive effect): Hydrocortisone suppresses the body’s natural response to injury or the presence of microbes like bacteria in the skin.
All about how topical hydrocortisone works
When we apply hydrocortisone to the skin, it enters skin cells. Inside the cells, it binds to the genetic material (DNA) and directs the cells to stop producing substances called prostaglandins and leukotrienes that cause inflammation. At the same time, hydrocortisone prevents the production of substances that attract inflammatory cells from the blood to the skin. The sum total of these effects is that hydrocortisone prevents and reduces inflammation.1
These functions make hydrocortisone a useful topical treatment for skin conditions such as:
- Insect bites
- Allergies
- Rash
- Eczema
- Dermatitis
- Itching2
Hydrocortisone is available in many forms, including ointments, creams, liquid solutions, sprays, or lotions. Typically, people apply hydrocortisone to the skin once or twice a day. Using it more frequently than that gives no improvement in results but does increase the risk of side effects.
All about different forms of hydrocortisone
Topical hydrocortisone can come in many different forms. The formulation used to deliver hydrocortisone to the skin is called the “vehicle.” Different vehicles are suited to different parts of the body. In addition, the type of vehicle can change how easily the skin can absorb the drug and therefore how effective it can be. Vehicles used for hydrocortisone include:
- Ointments: These formulations are best for dry or thick, callused lesions. They also work well for areas with thickened skin, such as the palms of the hands and soles of the feet. Ointments absorb well into the skin. However, they tend to be greasy, so they are inconvenient for hairy regions of the skin or for areas like the armpit.
- Creams: These water-based formulations are convenient because they vanish into the skin. However, they tend to dry the skin. Creams are generally less potent than ointments and do not penetrate into the skin as well as ointments do. Creams also typically contain preservatives, which can result in skin irritation and allergic reactions.
- Lotions: These formulations are alcohol-based. Thus, they work well for oozing cuts and lesions because they dry these out. Lotions are also convenient for hairy skin because they are non-greasy and leave no residue.
- Gels: These formulations are also non-greasy, making them convenient for the face as well as for hairy areas, where they cause no matting. However, gels may cause skin irritation.
- Foams and shampoos: These formulations are best for delivering steroids to the scalp. However, they tend to be more expensive.1,2
Hydrocortisone and Acne
So far, only one study has tested topical hydrocortisone as an acne treatment. The study showed that applying hydrocortisone to acne lesions does not help with acne.3
Expand to read details of study

The study was published in the journal Current Medical Research & Opinion in 1980. The researchers divided 50 people with mild-to-moderate acne into 2 groups:
- Group 1 applied a lotion containing hydrocortisone to the skin twice a day for the first 4 days, and then only once a day for 3 months.
- Group 2 applied a similar lotion without hydrocortisone to the skin following the same schedule.
The researchers examined the patients’ skin and counted acne lesions before, during, and after the course of treatment. Initially, acne seemed to be improving a little faster in Group 1, but this difference was not statistically significant, meaning it was so small it may have been due to random chance. By the end of treatment period, there was no difference in acne between the two groups, suggesting that the addition of hydrocortisone to the lotion did not help with acne.3
However, because hydrocortisone is easy to purchase without a prescription, many people do try treating their acne with it.
This study shows us that using hydrocortisone for acne may backfire
A group of dermatologists in India asked each of their patients whether they used topical steroids until they found 200 people who answered “yes.” The dermatologists then interviewed these patients and examined their skin.4
Out of the 200 people, it turned out that almost a third had been using the medication for their acne. Unfortunately, the researchers did not investigate whether the participants experienced any benefit from the medication. However, they did look at the patients’ skin for evidence of side effects and also asked the patients about any additional side effects they had experienced.4
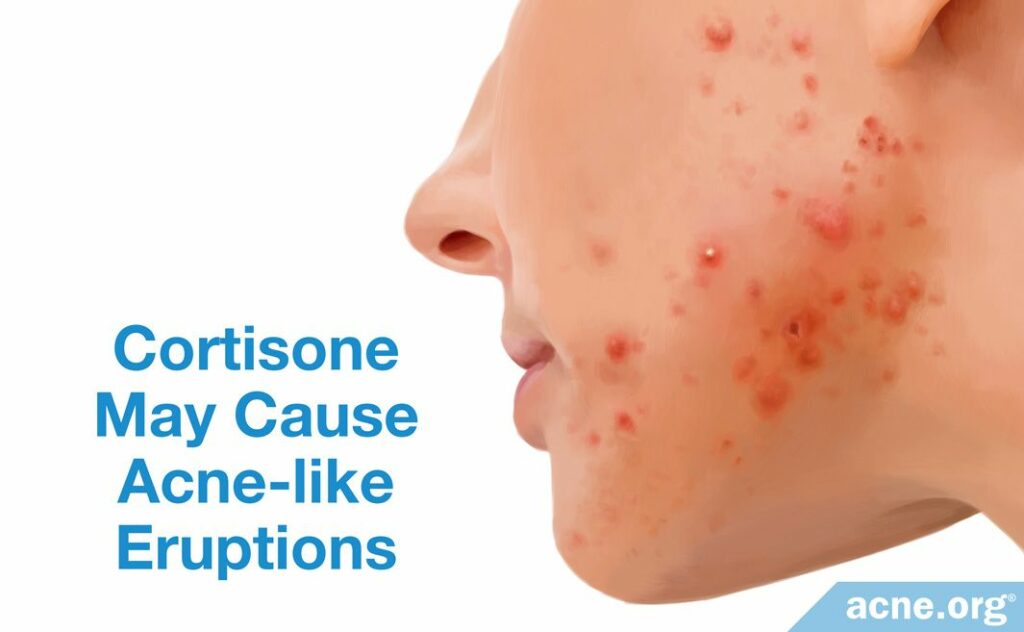
Ironically, the most common side effect of using topical steroids was the development of acne-like lesions (so-called acneiform eruptions). Almost a quarter of the study participants experienced this side effect.4
Expand to read details of study
The study was published in the Journal of Dermatologic Case Reports in 2017. The researchers interviewed 200 patients with various skin conditions who used topical steroids on their faces for more than 30 days. When asked the reason for using the drug, 59 patients or 29.5% replied that they were trying to cure their acne.4
The researchers also examined the patients and asked them what side effects they had experienced during the treatment. The most common side effect, reported by 23% of patients, was acneiform eruptions.4
We should note that the patients used many different topical steroids, and some patients applied more than one of the following to their skin at the same time:
- Betamethasone and clobetasol ointments: 75 patients or 37.5%
- Mometasone: 15 patients or 7.5%
- Kligman’s formula: 66 patients or 33%
- Combination medications containing some steroids: 54 patients or 27%3
Not only that, but all the patients used medications of different strengths. Since the researchers combined all the results, we cannot tell which specific medication caused which side effects. Finally, it is possible that some of the participants were simultaneously using other drugs or skincare products that may have contributed to the acneiform lesions.
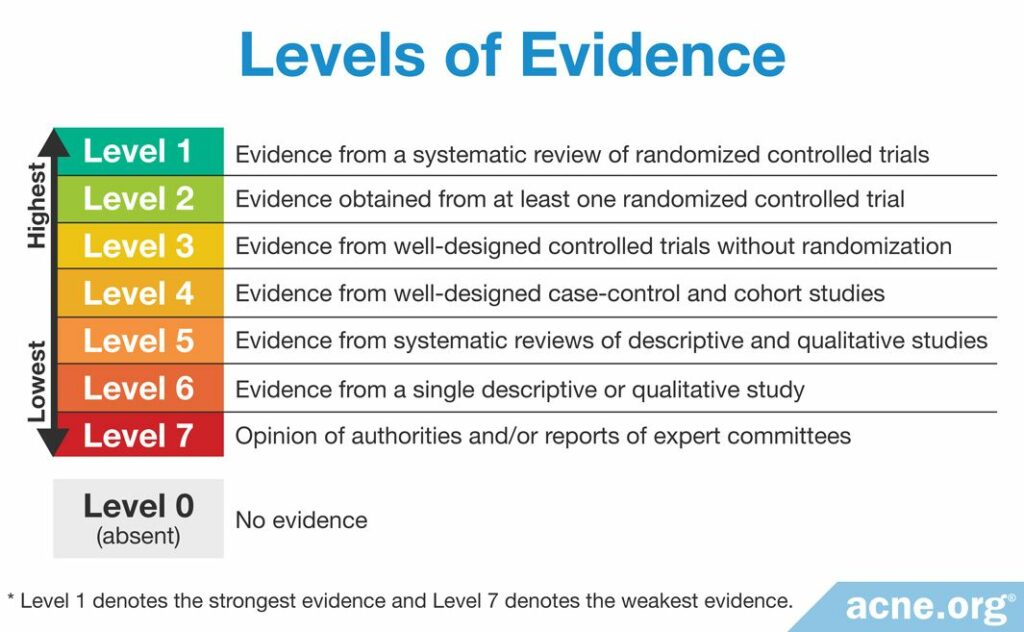
In other words, while this study provides the best information we have on the side effects of using topical steroids for acne, this evidence is relatively weak.
What Topical Hydrocortisone Does to the Skin
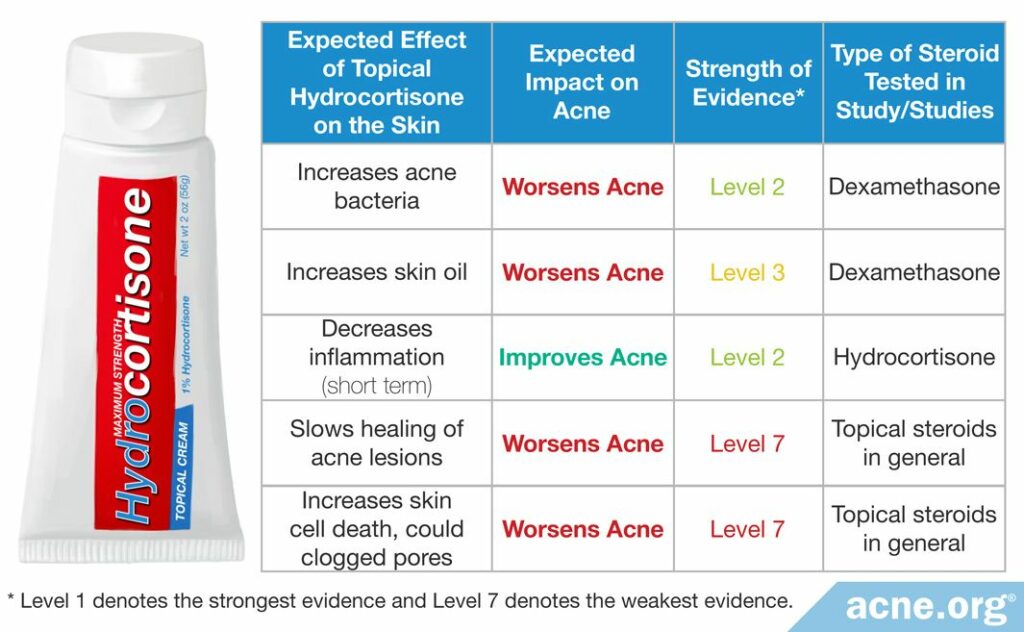
Since no studies have tested whether topical hydrocortisone helps with acne, we will have to look at what hydrocortisone does to the skin to figure out whether it would improve or worsen acne. The following table summarizes what this evidence suggests about how topical steroids likely act on the skin and what that means for acne.
The verdict on hydrocortisone for acne
Summing up the evidence, we can see that topical hydrocortisone is likely to intensify acne rather than improve it.
It is true that hydrocortisone may provide some relief in the short term by decreasing inflammation, which is a key part of acne. However, in the long run, the increased growth of bacteria, higher production of skin oil, slower healing of lesions, and increased clogging of pores by dead skin cells will probably make acne worse.
If you are curious to know more about the evidence on what steroids like hydrocortisone do to the skin, keep reading as we delve deeper into the science.
Topical Steroids May Boost the Growth of Acne Bacteria: The Evidence
Scientists agree that the acne bacteria called C. acnes play an important role in acne. When these bacteria overgrow in skin pores, they trigger inflammation, which is a major step on the path to developing acne. The bacteria also stimulate the skin to produce too many skin cells and too much skin oil, all of which contributes to acne.
One old study provides evidence that topical steroids like hydrocortisone boost the growth of these acne bacteria. In that study, 25 male participants applied a topical steroid to the forehead once a day for three weeks. The researchers examined the participants’ skin pores before and after the end of the treatment and counted the number of acne bacteria. They found that the number of acne bacteria in the skin pores increased significantly after using the topical steroid. The researchers wrote, “[The treatment] led to an increase in bacterial count for C. acnes.”5
This result suggests that applying topical steroids like hydrocortisone to the skin for several weeks may increase the growth of acne bacteria and lead to a worsening of acne. However, we should keep in mind that the participants in this study used dexamethasone instead of hydrocortisone. While the two drugs are related, dexamethasone is almost 40 times more potent and longer-acting. This means you need to apply 40 times more hydrocortisone to achieve the same effect. You also need to apply hydrocortisone more often to get the same results as with dexamethasone. Because of its potency, dexamethasone is only available by prescription.
In other words, hydrocortisone may not boost the growth of bacteria nearly as much as the dexamethasone in this study. Then again, because hydrocortisone is a weaker drug, patients may just end up applying more hydrocortisone and using it more frequently, leading to the same end result.
Expand to read details of study

The study was published in the European Journal of Clinical Pharmacology in 1978. Twenty-five healthy males participated in the study. The topical steroid was a preparation of 0.02% dexamethasone in a common skincare ingredient called Eutanol G. The participants applied this steroid treatment to the right side of the forehead once a day for three weeks. At the same time, they applied just Eutanol G to the left side of the forehead for comparison. The researchers removed bacteria from the participants’ skin pores before the beginning of treatment and at the end of three weeks. They found an increase in the number of C. acnes and other bacteria on the side of the forehead treated with dexamethasone, but not on the side treated with just Eutanol G.5
Topical Steroids May Increase the Production of Skin Oil: The Evidence
Excessive production of skin oil is one of the causes of acne. Too much skin oil can clog pores and lead to the early stages of acne.
One study has looked at how topical steroids change the production of skin oil. Like the previous study, this one tested dexamethasone rather than hydrocortisone, so again, we cannot necessarily assume that hydrocortisone would have exactly the same effects.
In that study, 16 healthy teenage boys applied dexamethasone to the back twice every day for 26 days. After this period, the researchers analyzed skin oil from the boys’ backs. They found that the steroid treatment changed the skin oil, so that it contained more oily components (free fatty acids) and less body fats (triglycerides). The researchers conjectured that this increase in oily components made acne more likely to develop. They wrote, “One may thus assume that the increase in free fatty acids which we have demonstrated can induce [clogged pore] formation under steroid treatment.”6
Expand to read details of study

The study was published in the journal Archives of Dermatological Research in 1978. The participants were 16 teenage boys between the ages of 13 and 16 with no skin conditions. The boys applied a fat- and oil-free treatment containing 0.05% dexamethasone to the right side of the back and the same product but lacking dexamethasone to the left side of the back. The treatment continued twice a day for 26 days. Two days after the end of treatment, the researchers extracted skin oil from each boy’s back and analyzed it. They found a change in the composition of skin oils from the right side of the back, but no change in skin oil from the left side.6
Topical Steroids May Decrease Skin Inflammation in the Short Term: The Evidence
As we have already mentioned, acne is an inflammatory disease. Inflammation around the glands that produce skin oil is a key part of how acne begins and gets worse. Therefore, a treatment that reduces inflammation should help with acne.
One of the ways that hydrocortisone prevents skin inflammation is by making blood vessels narrower (vasoconstriction), which stops inflammatory cells from the blood from reaching the skin. When the blood vessels become narrower, the skin turns pale, which doctors call “blanching.”
One study looked at blanching in 10 volunteers who applied hydrocortisone cream to the arm twice a day for 5 days. As expected, the researchers found significant blanching in the volunteers’ skin after only a few days. They also noticed that the effect was additive: in other words, the blanching became stronger with repeated treatment.7 This means that the blood vessels in the arm became narrower, presumably leading to decreased inflammation. The volunteers in this study were acne-free, but if they had had acne, perhaps they would have experienced a temporary improvement in their breakouts.
Interestingly, the researchers found that the skin returned to its normal, non-blanched color one day after the volunteers stopped treatment. In other words, we can assume that the anti-inflammatory effect of the hydrocortisone cream is short-lived.
Expand to read details of study

The study was published in the Australasian Journal of Dermatology in 2015. Ten volunteers participated in the study. The researchers tested two different hydrocortisone creams: a 1% dissolved hydrocortisone cream and a 1% dispersed hydrocortisone cream. The volunteers applied the first cream to two locations on the forearm and the second cream to two other locations on the forearm. The experiment was double-blind, which means neither the researchers nor the volunteers knew which cream was placed on which locations until the end of the experiment. The participants applied each cream twice a day for 5 days. The scientists measured skin blanching before the start of the experiment, then 3 times a day for 6 days, and once at the end of 7 days. They found that both creams caused significant blanching, but the dissolved hydrocortisone cream was more effective than the dispersed hydrocortisone cream. None of the volunteers experienced side effects.7
Topical Steroids May Slow the Healing of Acne Lesions: The Evidence
In a medical sense, acne lesions are wounds. Most acne lesions are closed wounds, but a popped or picked pimple becomes an open wound. Either way, the healing of acne lesions is a type of wound healing.
Doctors avoid applying steroids to open wounds. The theory is that steroids prevent new skin cells from growing, which is a problem because new cells are needed to close the wound and repair the damage. In addition, research suggests that hydrocortisone slows down the formation of new collagen, which is an important component of rebuilding the skin at the wound site.8 Not only that, doctors worry that applying steroids like hydrocortisone to an open wound will result in the body absorbing too much of the drug. If the drug ends up in the blood, it will circulate throughout the body, causing side effects in multiple organs (so-called systemic side effects).9
In other words, the medical community believes that hydrocortisone slows down the healing of wounds, including acne lesions. Doctors also consider it a bad idea to apply hydrocortisone to breaks in the skin because of the risk of whole-body side effects.
Topical Steroids May Increase the Death of Skin Cells: The Evidence
Researchers believe that not only do topical steroids prevent new skin cells from growing, but they also increase the number of skin cells dying at any given time. More dead skin cells piling up means a higher likelihood of clogged skin pores. Clogged pores, or comedones, are the first stage of acne lesions.9 However, at this point we have no direct evidence that topical medications like hydrocortisone really lead to more clogged pores and more acne.
Summing up the evidence, there are multiple good reasons to avoid treating acne with topical hydrocortisone and only one reason to think the drug could actually help. On balance, it is probably wise to leave this treatment on the drugstore shelf.
It is also important to be aware of potential side effects when considering any treatment.
Side Effects of Topical Hydrocortisone
Known side effects of hydrocortisone on the skin include:
- Burning
- Itching
- Irritation
- Redness
- Dryness10
Using hydrocortisone for a prolonged period or on large areas of the body can lead to additional side effects:
- Development of acne or acneiform lesions
- Unwanted growth of body hair
- Darkening or lightening of the skin
- Susceptibility to skin infections
- Contact dermatitis (an allergic skin rash)
- Rosacea (a chronic skin condition involving a flushed face with red lesions)11-14
Fortunately, most of these side effects are temporary and disappear when the person stops using the drug.
Whole-body (systemic) side effects are possible if the body absorbs a large amount of hydrocortisone. This may occur after using hydrocortisone on large areas for a long period of time, such as for body acne. Such side effects are rare and mostly occur in people using high-potency steroids for severe skin diseases. Whole-body side effects may include:
- Weight gain, especially around the face, upper back, and torso
- Delayed healing of wounds
- Irregular menstrual period
- Changes in sexual function
- Muscle weakness1
Unfortunately, many people with acne self-medicate with hydrocortisone and are therefore prone to suffering from its side effects.

According to a 2016 article in the Indian Journal of Dermatology, misuse of hydrocortisone is common among acne patients, including on the advice of a pharmacist or doctor. The article authors wrote, “Misuse of topical steroids not just over the face but also as a cream for any skin problem is quite common…It is very important to [educate] these people about the possible complications of these drugs.”13
The History of Hydrocortisone
Scientists first isolated hydrocortisone from the adrenal glands of cows in 1948. In 1952, researchers first demonstrated that hydrocortisone could be effective in treating skin conditions. Since then, hydrocortisone has become a popular topical treatment. Because it is available over-the-counter, people tend to misuse it.1
The Bottom Line
Although topical hydrocortisone is available without a prescription and may help reduce inflammation in the short term, the evidence we have suggests that it is ultimately more likely to worsen acne than to improve it.
Furthermore, its long-term use can cause serious unwanted side effects.
Therefore, it is best to avoid it as an acne treatment.
References
- Gautam, M. et al. Topical corticosteroids in dermatology. Indian J. Dermatology, Venereol. Leprol. 82, 371 (2016). https://www.ncbi.nlm.nih.gov/pubmed/27279294
- Ference, J. D. & Last, A. R. Choosing Topical Corticosteroids. 79, (2009). https://www.ncbi.nlm.nih.gov/pubmed/19178066
- Guerrier, C. J. & Thornton, E. J. Double-blind comparison of two similar lotion formulations, one without and the other with hydrocortisone acetate (‘Actinac’) in the treatment of acne vulgaris. Curr. Med. Res. Opin. 6, 377-379 (1980). https://pubmed.ncbi.nlm.nih.gov/6444861/
- Sharma, R., Abrol, S. & Wani, M. Misuse of topical corticosteroids on facial skin. A study of 200 patients. J. Dermatol. Case Rep. 11, 5 – 8 (2017). https://www.ncbi.nlm.nih.gov/pubmed/28539982
- Gloor, M., Funder, H. & Franke, M. Effect of topical application of dexamethasone on propionibacteria in the pilosebaceous duct. Eur. J. Clin. Pharmacol. 14, 53 – 56 (1978). https://www.ncbi.nlm.nih.gov/pubmed/729607
- Gloor, M. & Mildenberger, K. H. Influence of an external therapy with dexamethasone-21-sodium-M-sulfobenzoate on the amount of free fatty acids in the skin surface lipids. Arch. Dermatol. Res. 261, 33 – 38 (1978). https://link.springer.com/article/10.1007/BF00455373
- Greive, K. A. & Barnes, T. M. Increased bioavailability of hydrocortisone dissolved in a cream base. Australas. J. Dermatol. 56, 30 – 34 (2015). https://www.ncbi.nlm.nih.gov/pubmed/24372079
- Haapasaari, K. M., Risteli, J., Koivukangas, V. & Oikarinen, A. Comparison of the effect of hydrocortisone, hydrocortisone-17-butyrate and betamethasone on collagen synthesis in human skin in vivo. Acta Derm. Venereol. 75, 269-271 (1995). https://pubmed.ncbi.nlm.nih.gov/8578945/
- Abraham, A. & Roga, G. Topical steroid-damaged skin. Indian J. Dermatol. 59, 456 – 459 (2018). https://www.ncbi.nlm.nih.gov/pubmed/25284849
- Uva, L. et al. Mechanisms of action of topical corticosteroids in psoriasis. Int. J. Endocrinol. 2012, (2012). https://www.ncbi.nlm.nih.gov/pubmed/23213332
- Meena, S. et al. Topical corticosteroids abuse: A clinical study of cutaneous adverse effects. Indian J. Dermatol. 62, 567 (2017). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5724325/
- Coondoo, A., Phiske, M., Verma, S. & Lahiri, K. Side-effects of topical steroids: A long overdue revisit. Indian Dermatol Online J. 5, 416-425 (2014). https://pubmed.ncbi.nlm.nih.gov/25396122/
- Nagesh, T. S. & Akhilesh, A. Topical steroid awareness and abuse: A prospective study among dermatology outpatients. Indian J. Dermatol. 61, 618-621 (2016). https://pubmed.ncbi.nlm.nih.gov/27904178/
- Fisher, D. A. Adverse effects of topical corticosteroid use. West. J. Med. 162, 123-126 (1995). https://pubmed.ncbi.nlm.nih.gov/7794369/
The post Can Topical Hydrocortisone Help with Acne? appeared first on Acne.org.